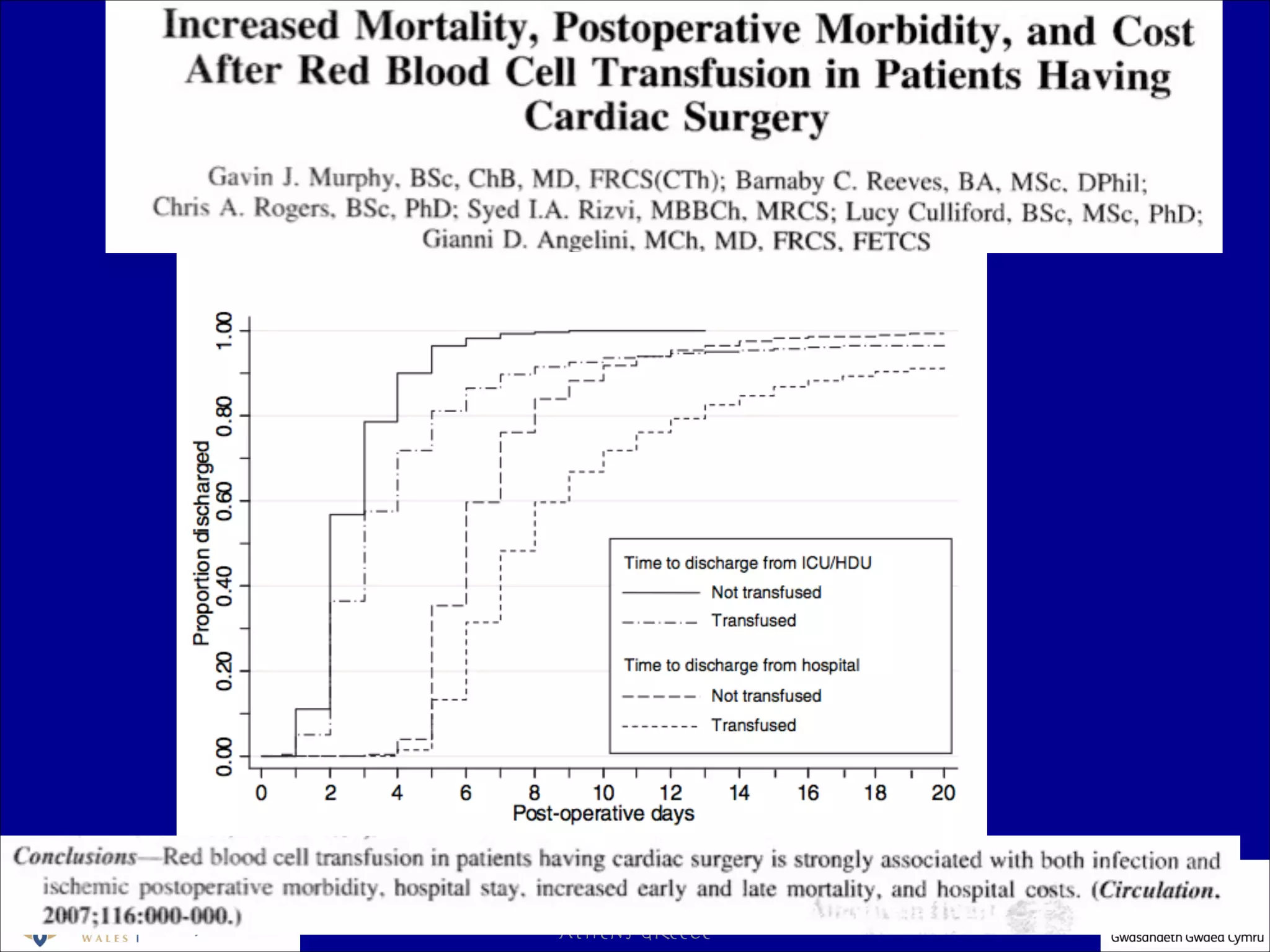
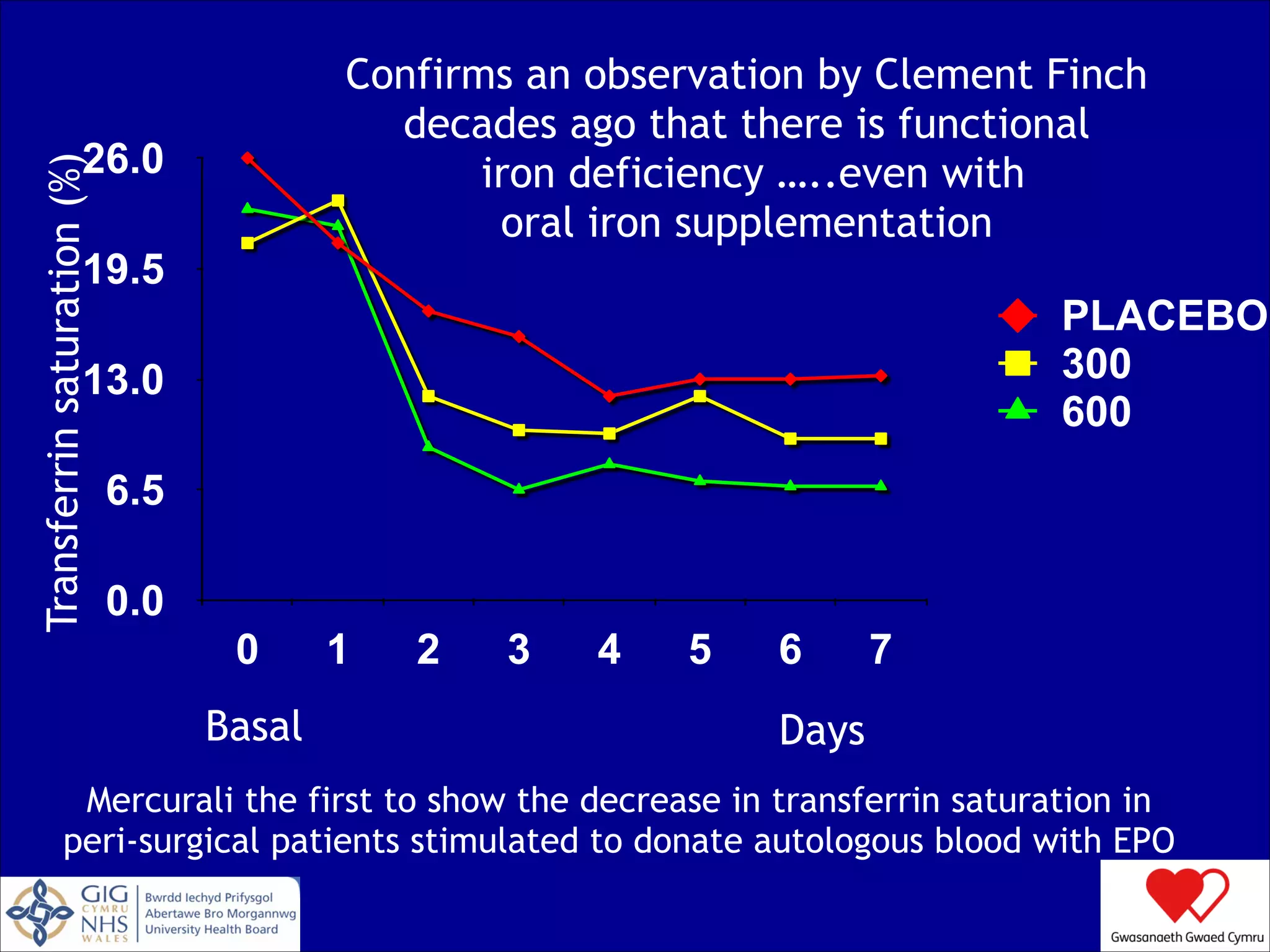
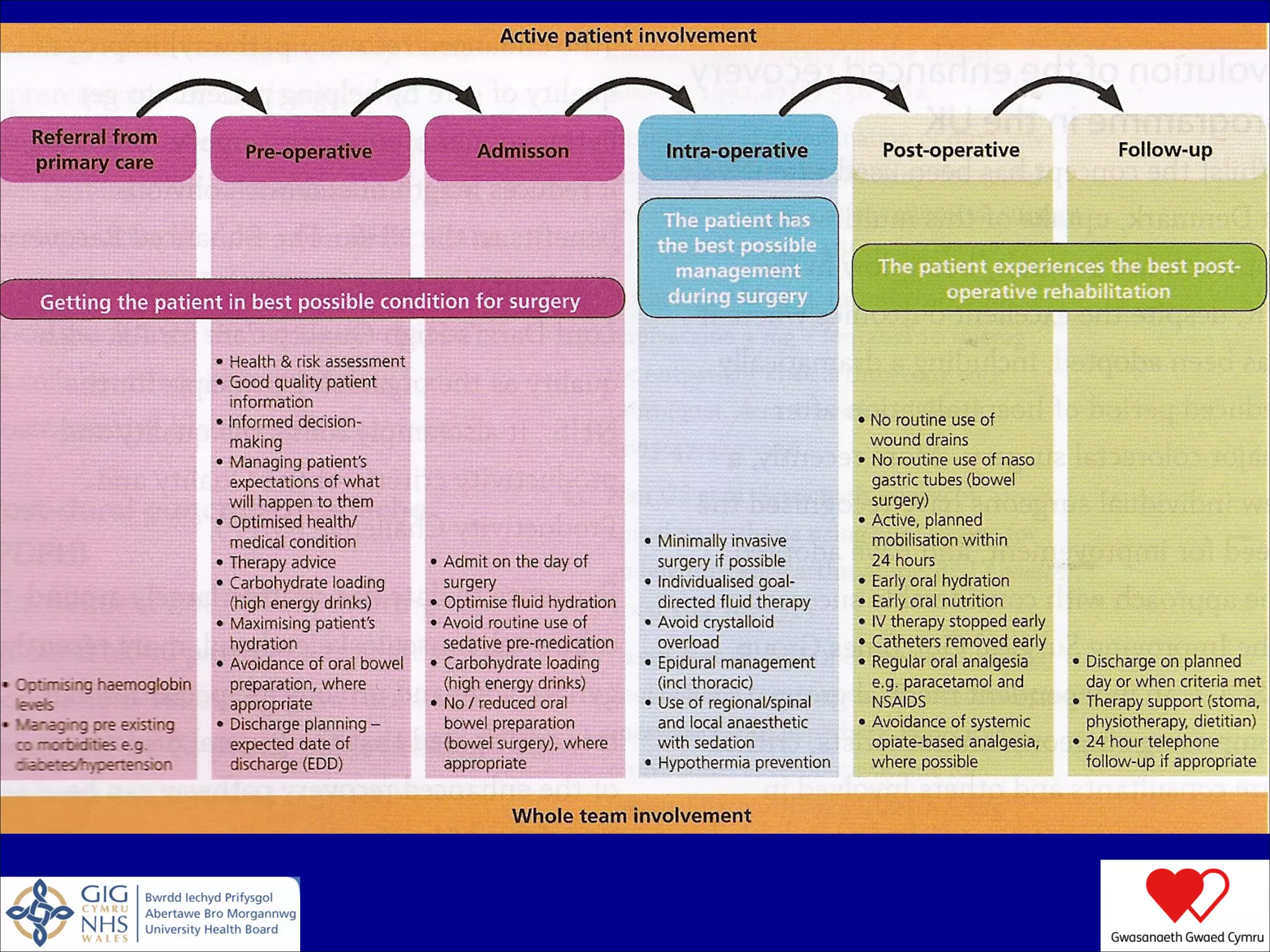
The document discusses blood conservation strategies in transfusion medicine, highlighting the importance of patient blood management (PBM) principles to optimize and minimize the use of allogeneic blood. It emphasizes integrating transfusion alternatives, preoperative assessment, and planning to improve patient outcomes while addressing potential risks associated with blood transfusions. The author, Dafydd Thomas, advocates for a paradigm shift in transfusion practices, focusing on the patient's needs and safety over the traditional product-centric approach.