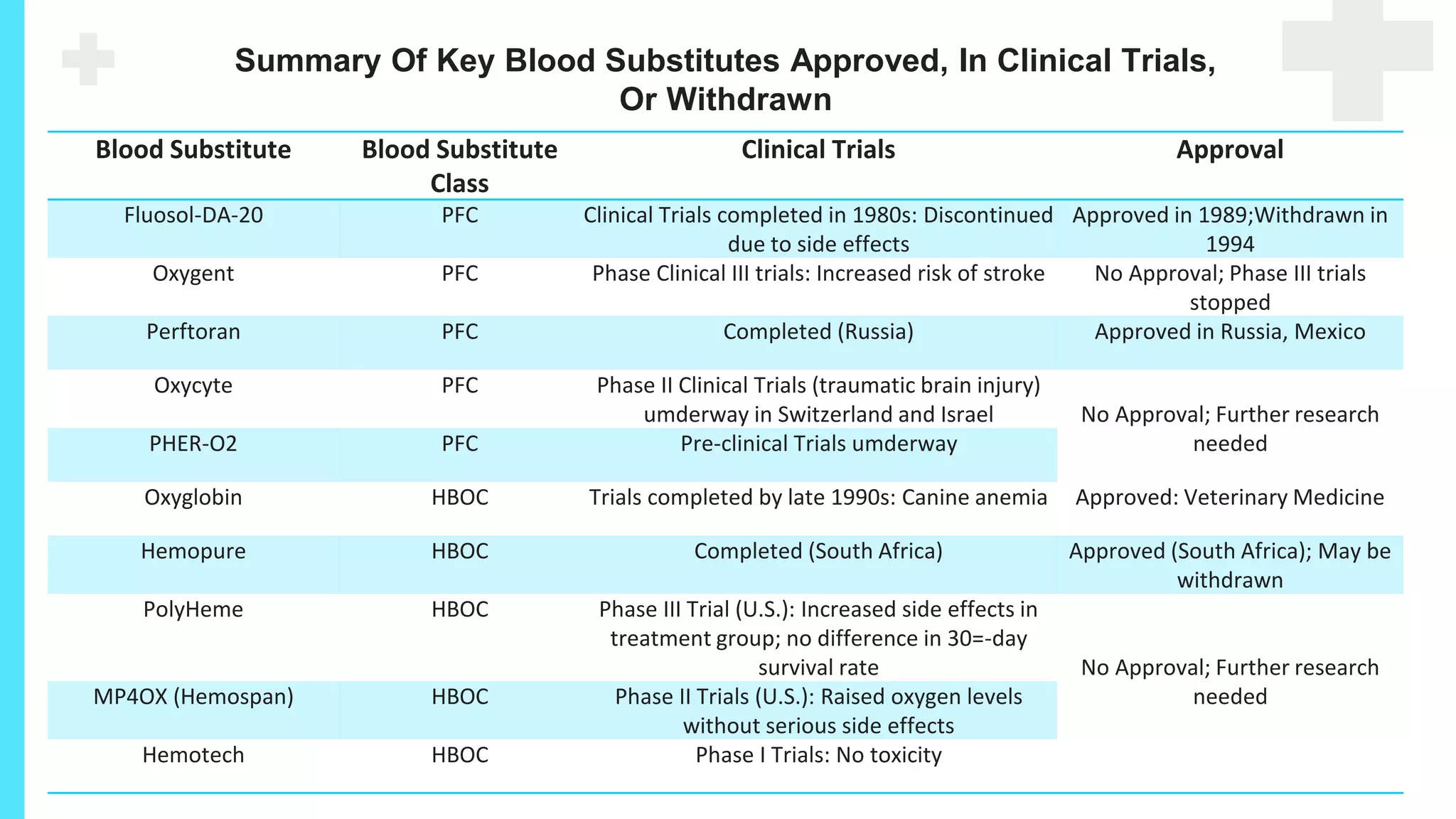
There are several alternatives to blood transfusion that can help reduce its use and risks. These include treating pre-existing anemia, using medications to stimulate red blood cell production or stop bleeding, employing blood-saving surgical techniques and technologies like cell salvage machines. While blood substitutes have been studied, none have gained approval due to safety issues. Implementing strategies of patient blood management can help minimize allogenic blood transfusions.



































![First-Generation
Perfluorocarbon emulsions
Fluosol-DA
Oxygent
Oxycyte
- FDA approved for percutaneous
transluminal coronary angioplasty.
- Withdrawn from the market:
A short effective half-life
Low oxygen-carrying capacity
Acute complement activation
Phase III trials -
increased incidence
of stroke and trials
have been halted.[6]
Entering phase II trials](https://image.slidesharecdn.com/alternativestobloodtransfusion-230918181814-19e360f4/75/ALTERNATIVES-TO-BLOOD-TRANSFUSION-pptx-36-2048.jpg)