Embed presentation
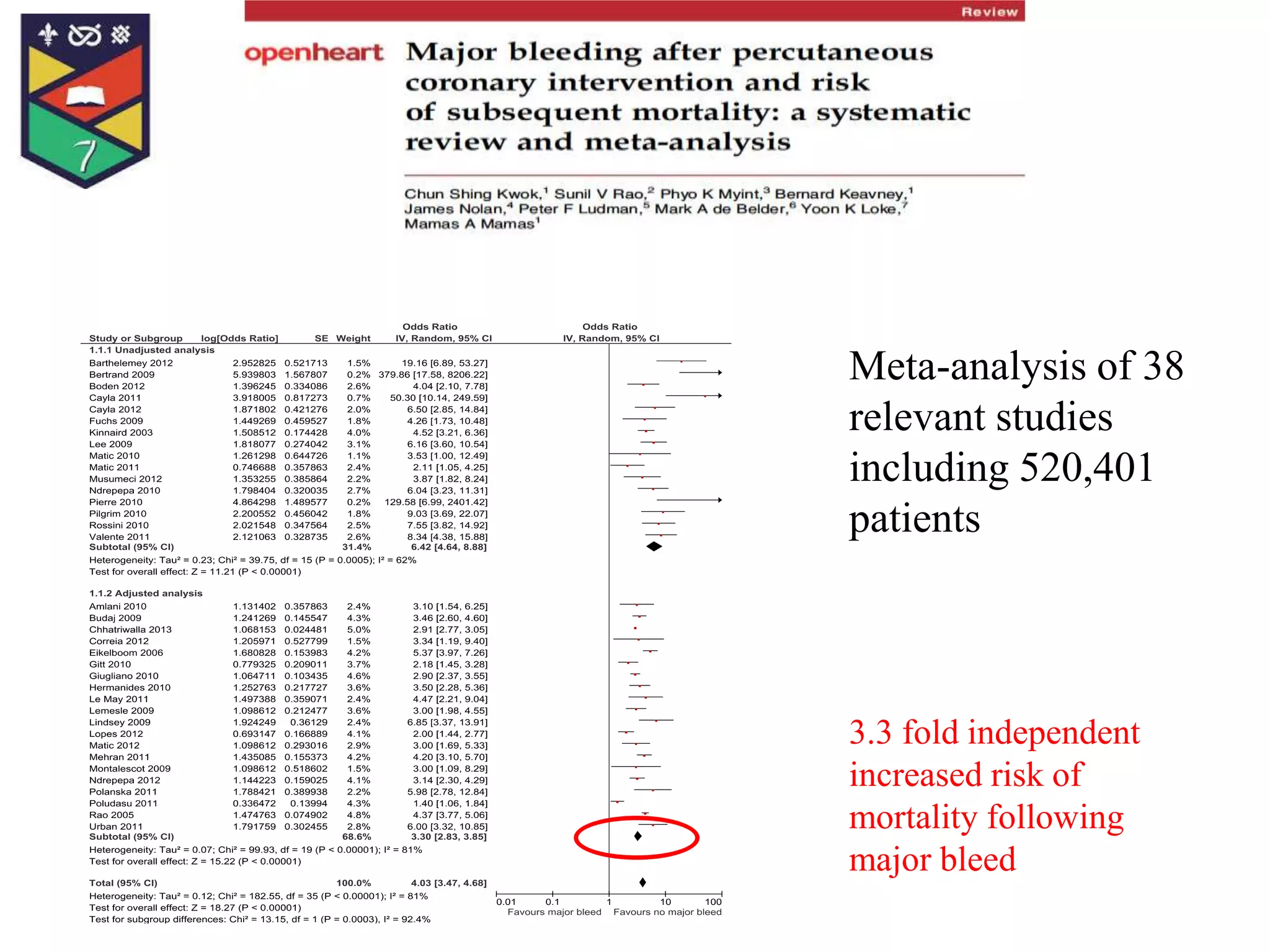
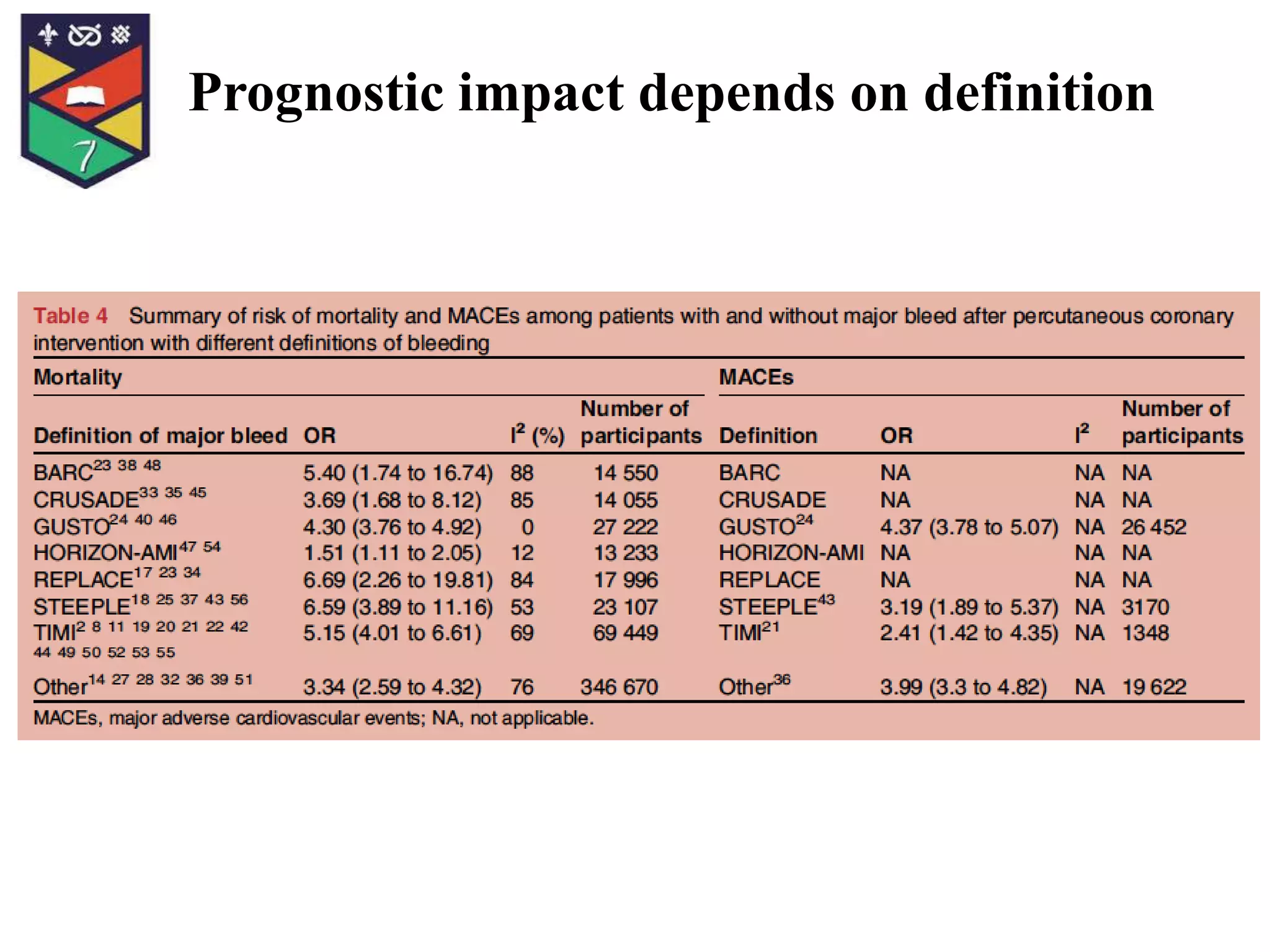
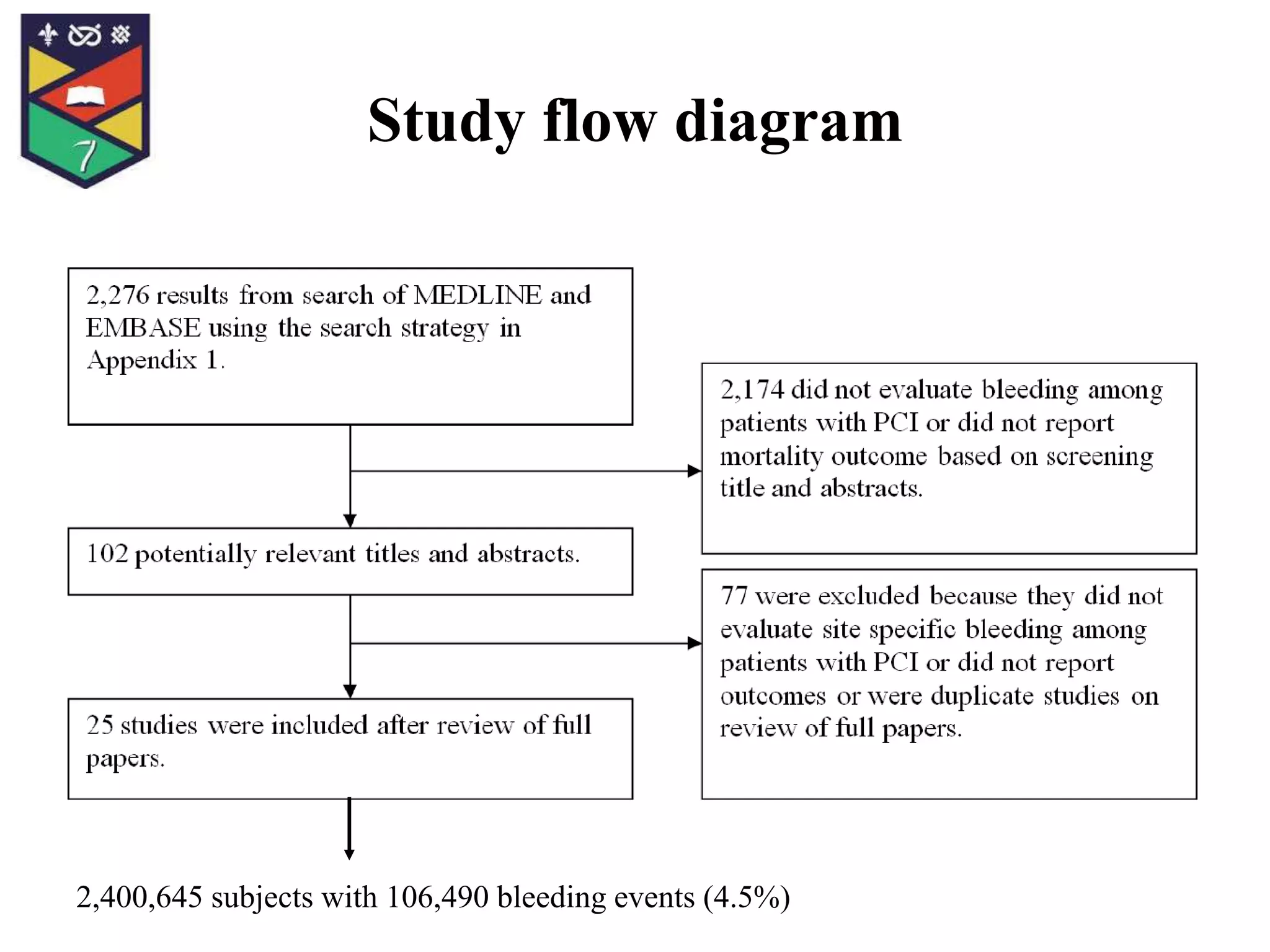
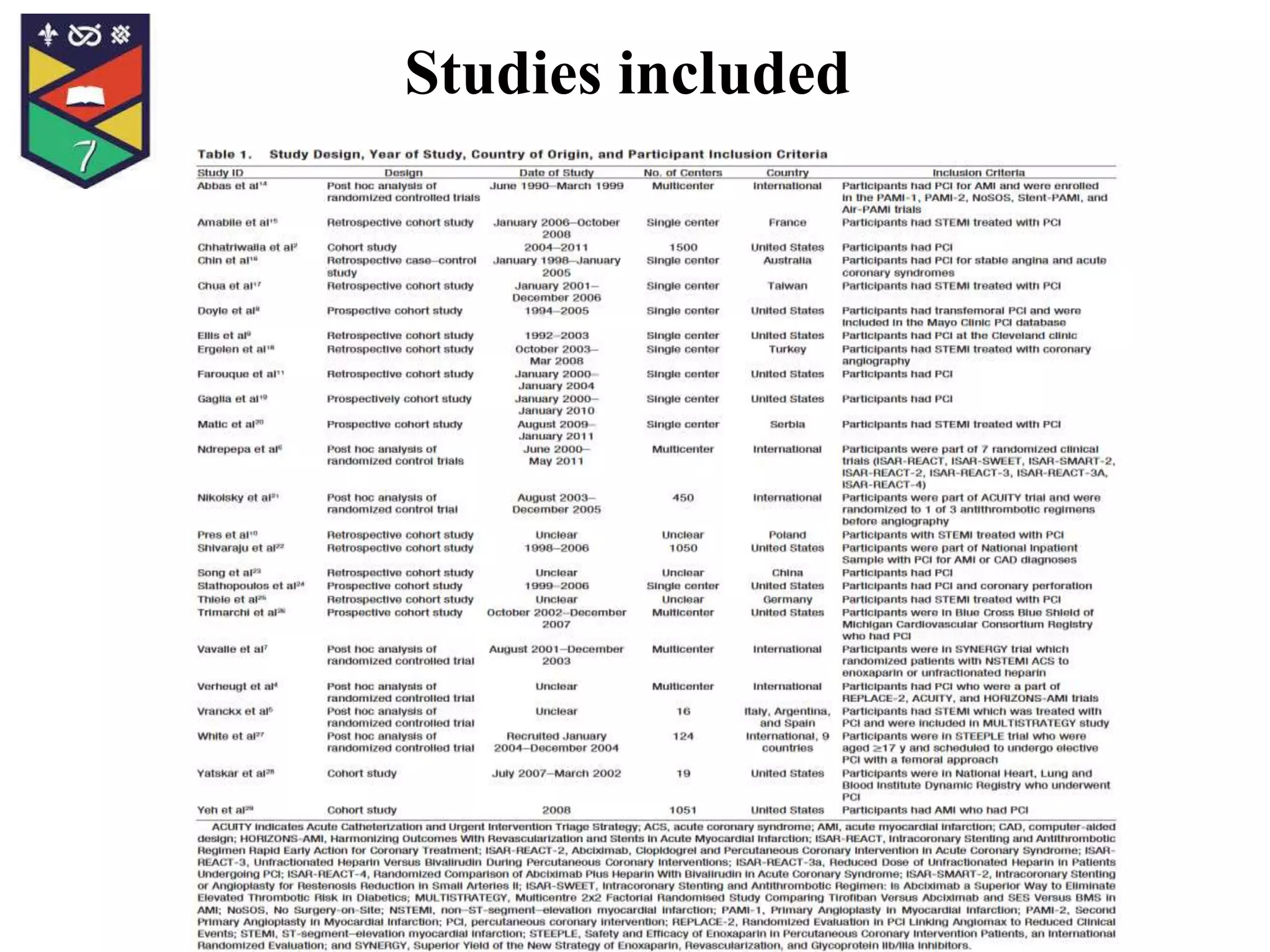
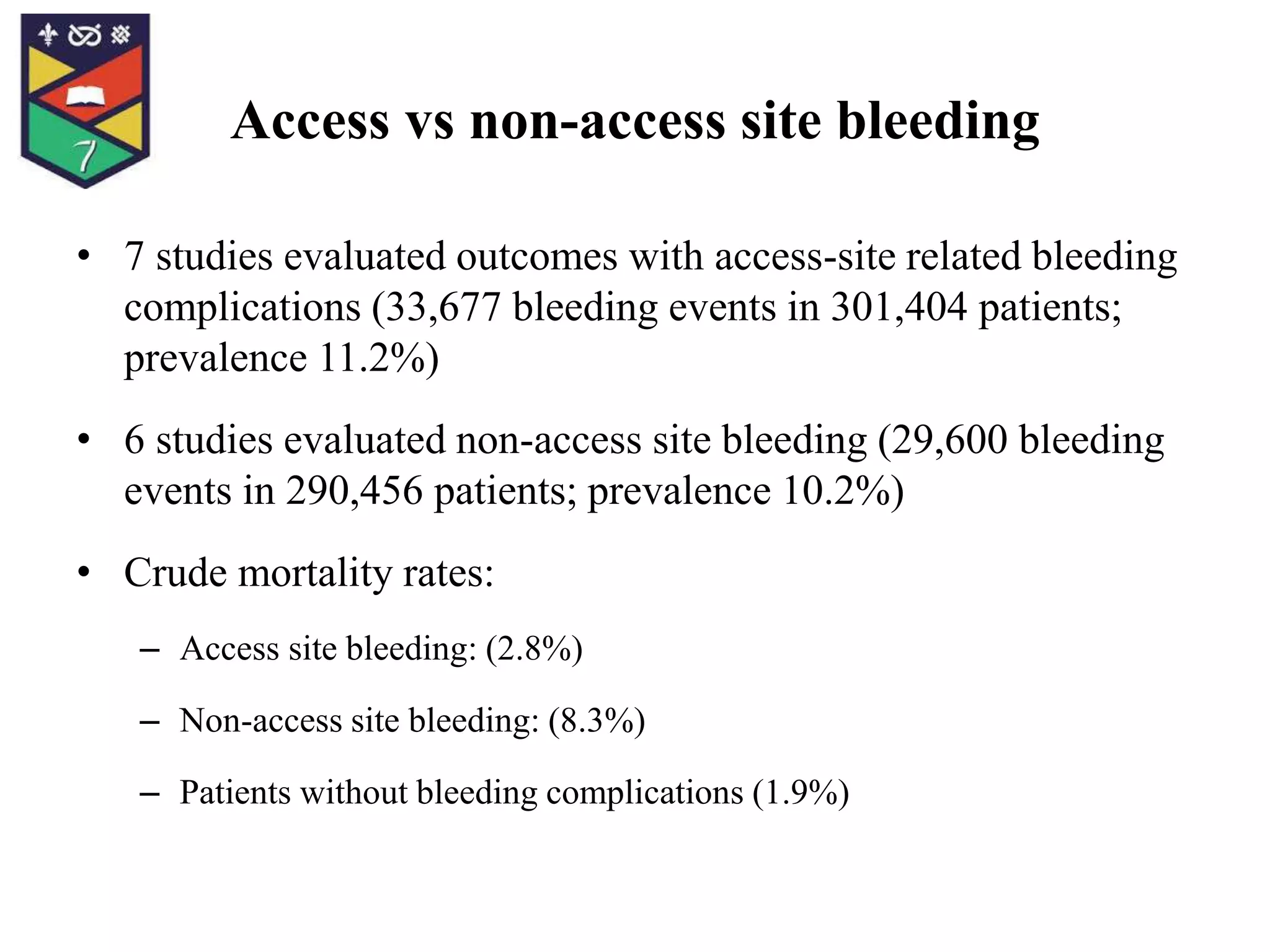
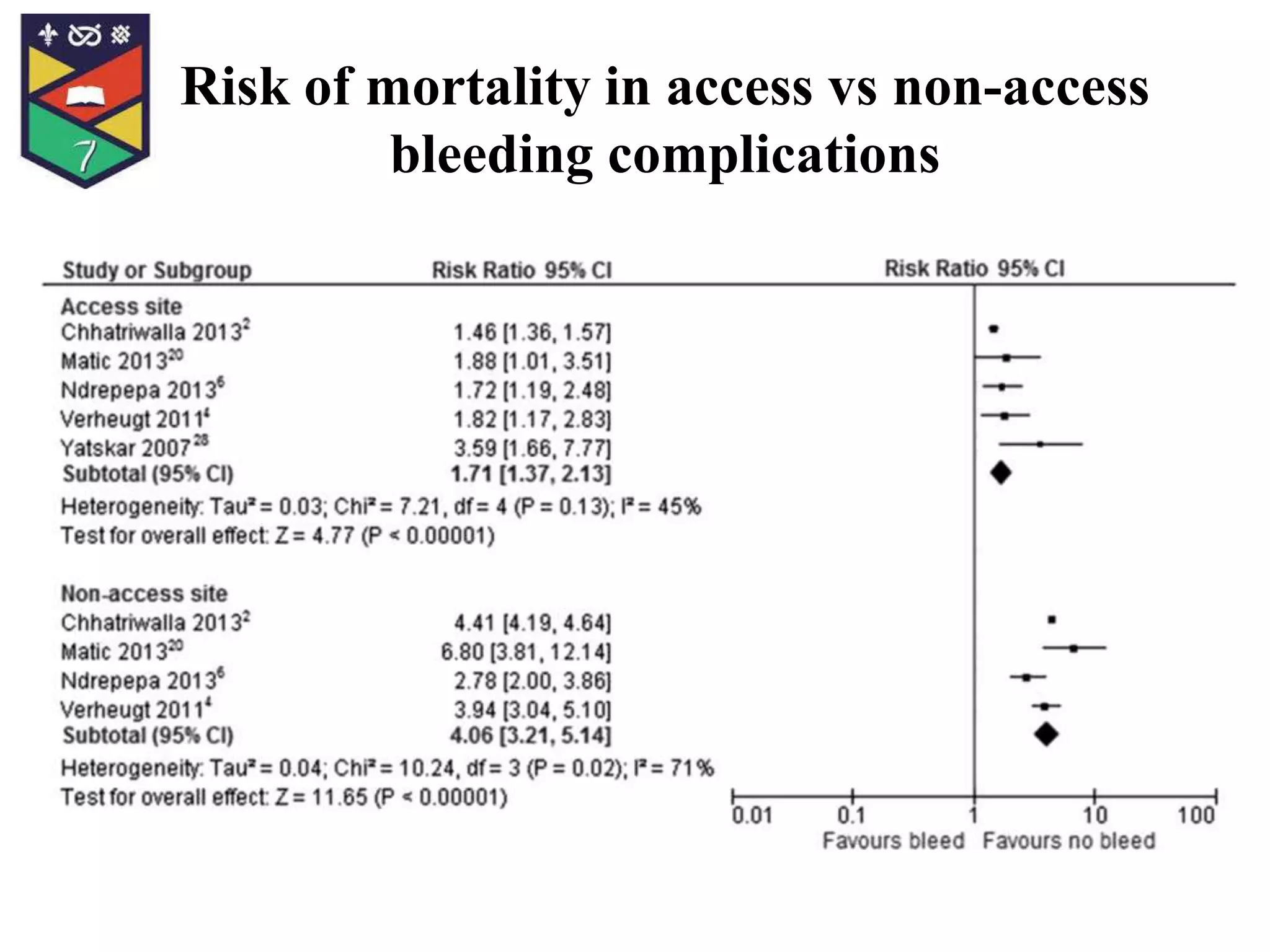
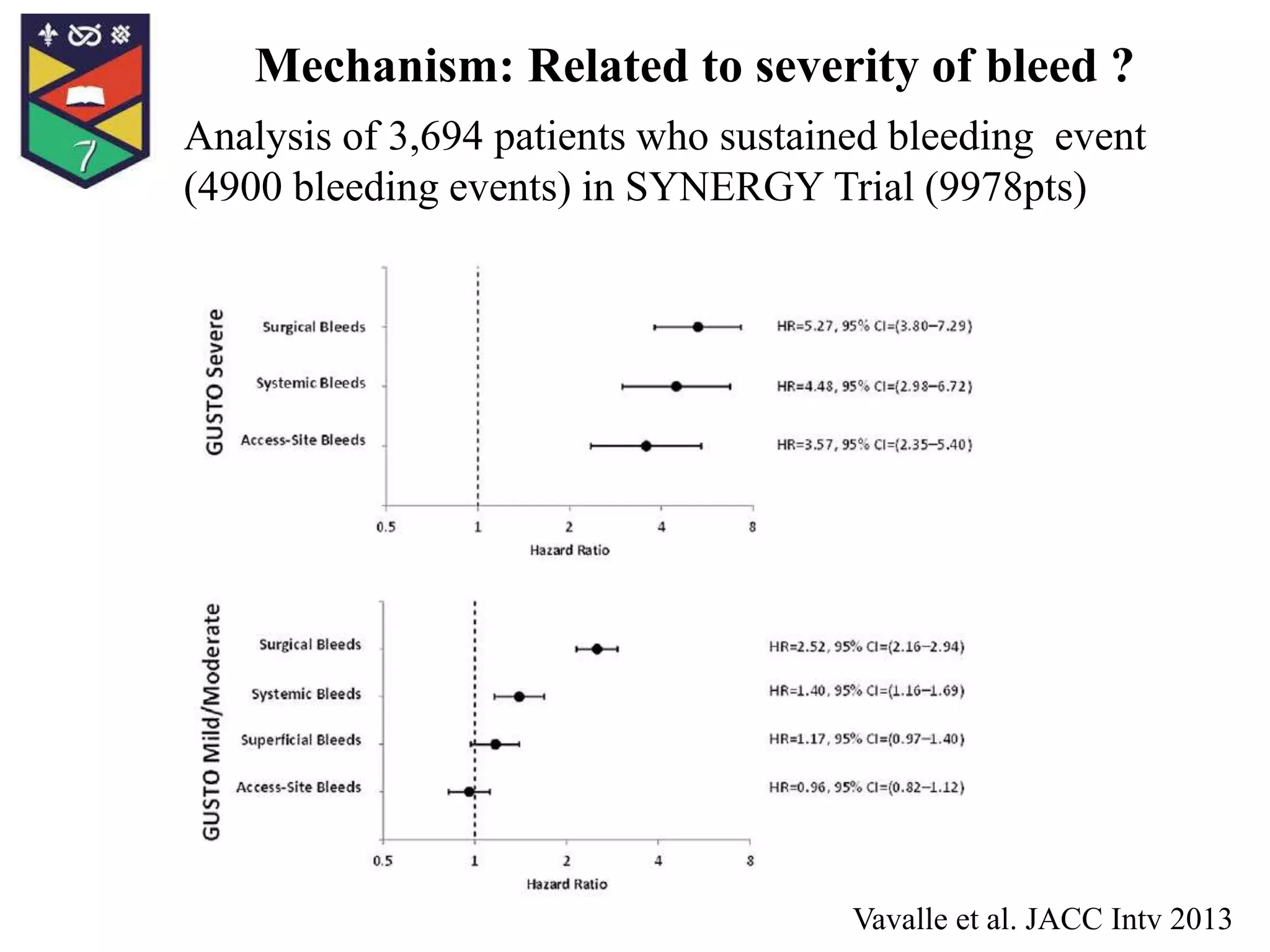
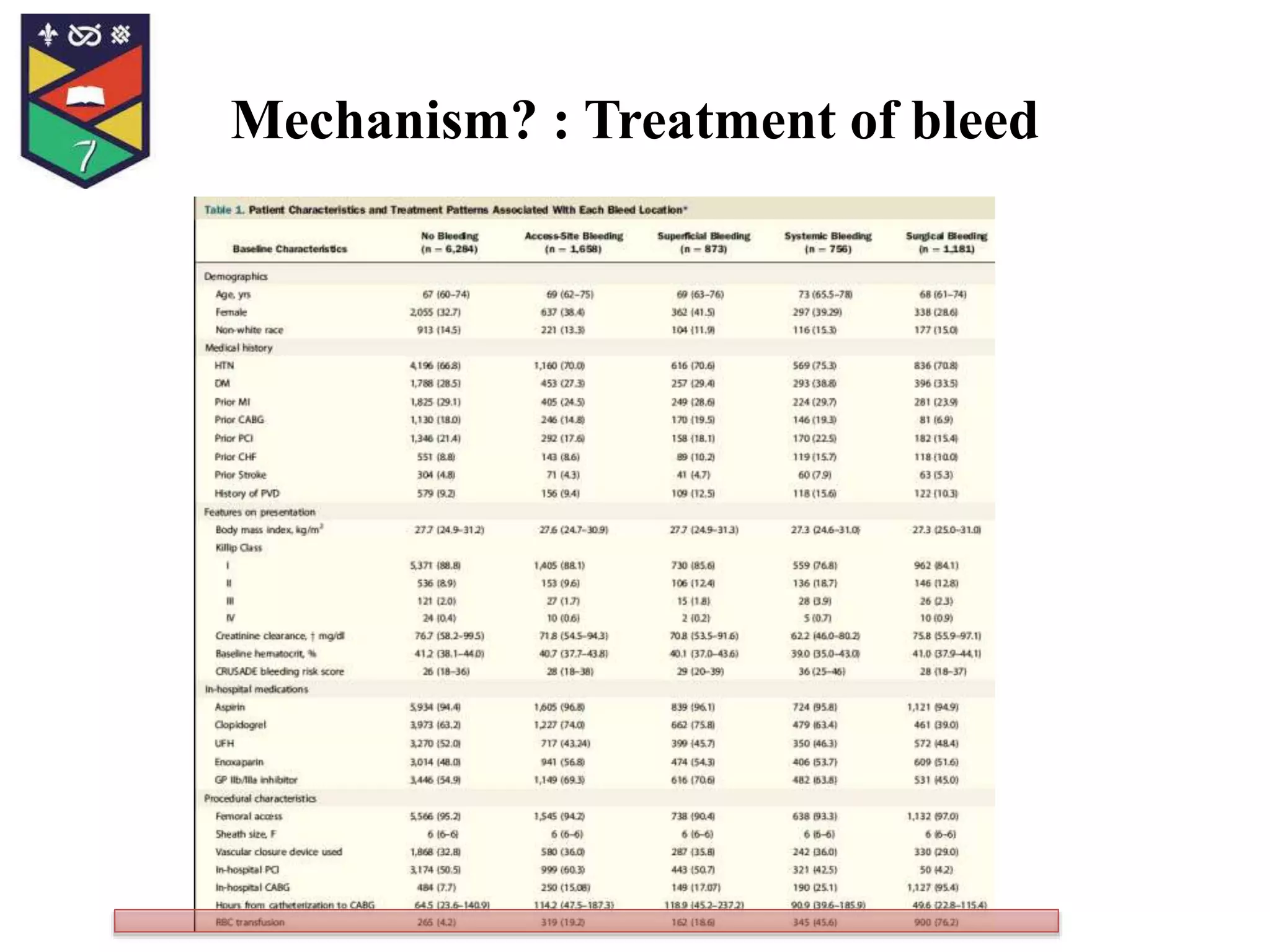
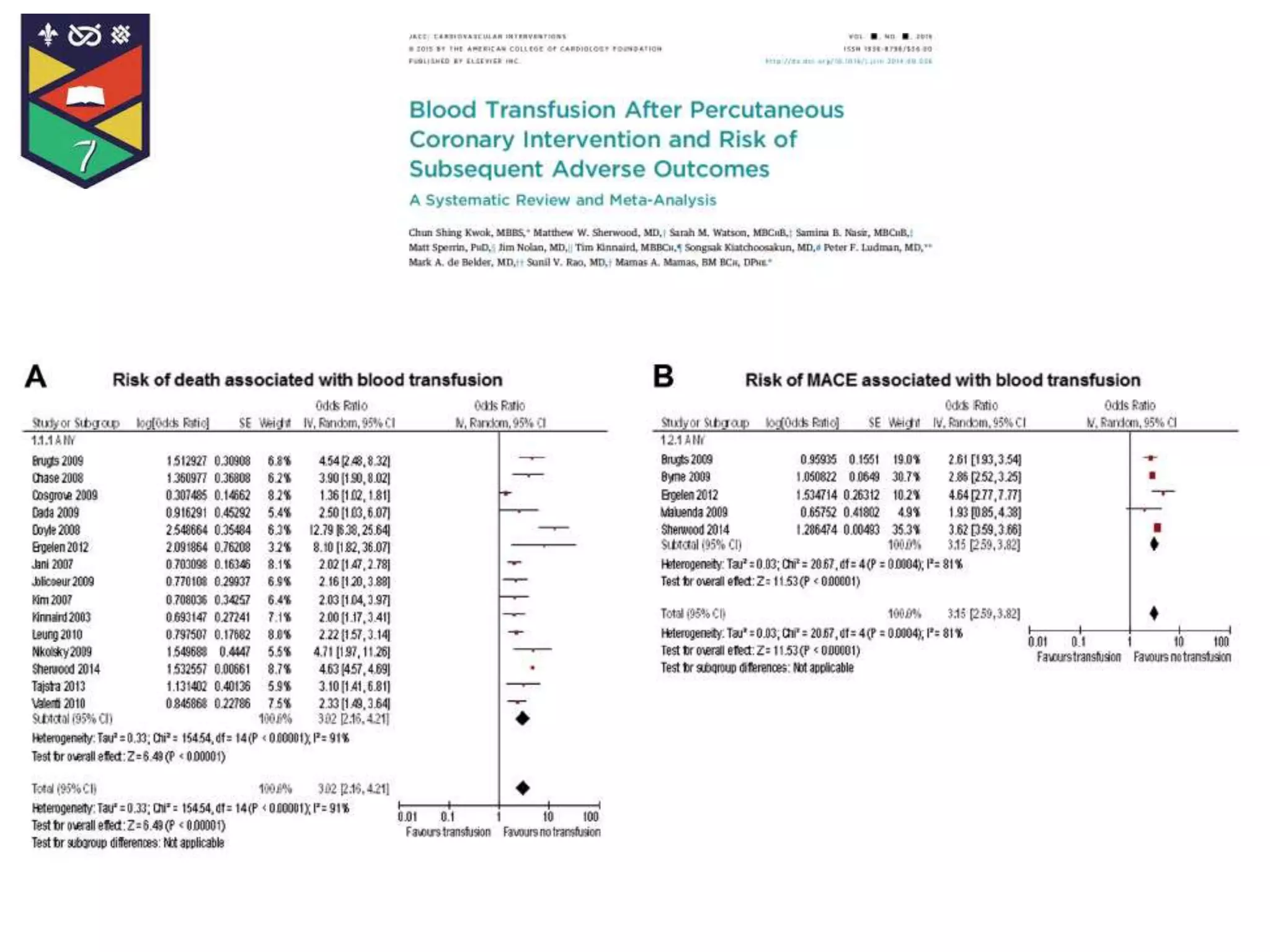
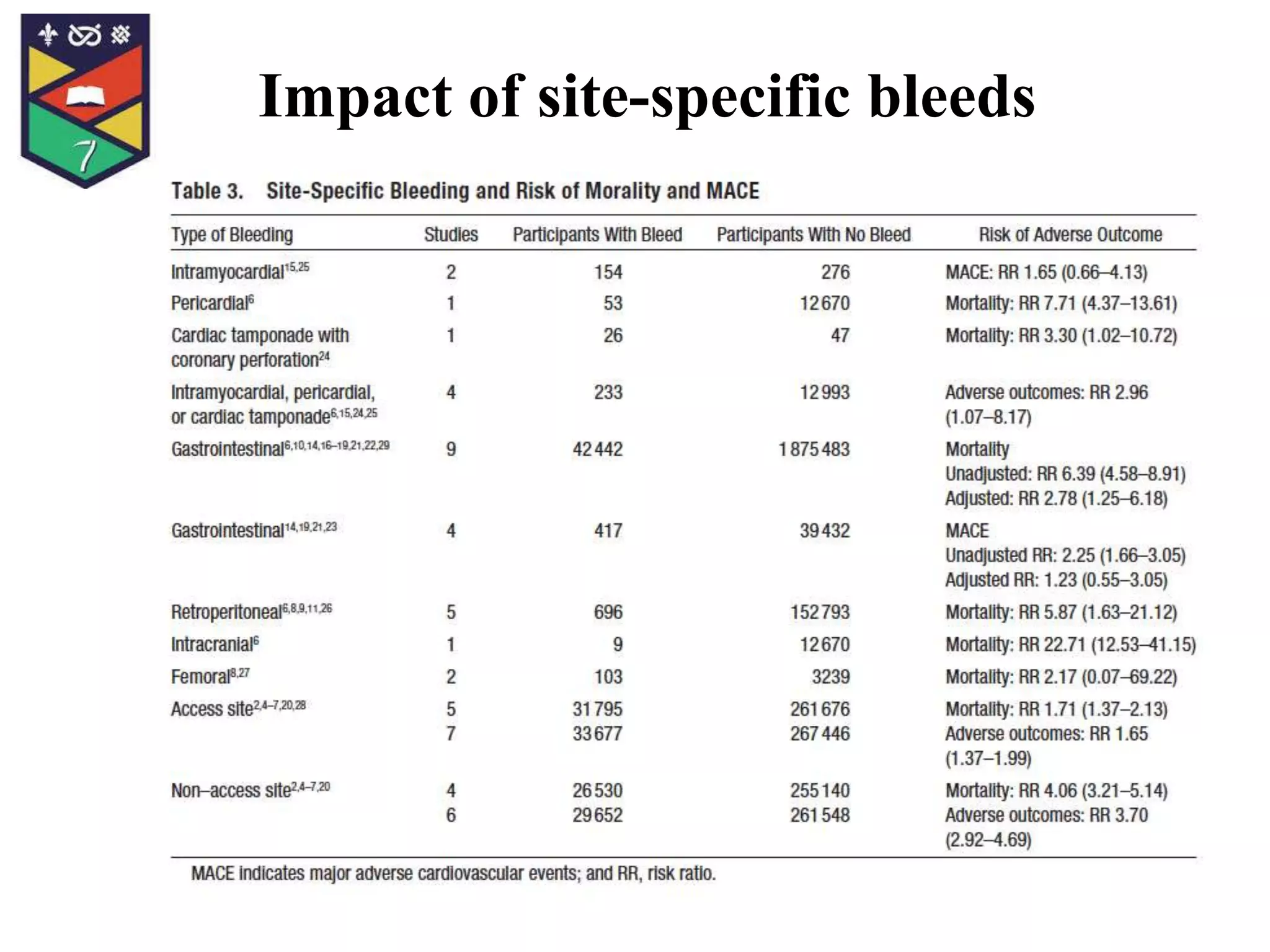
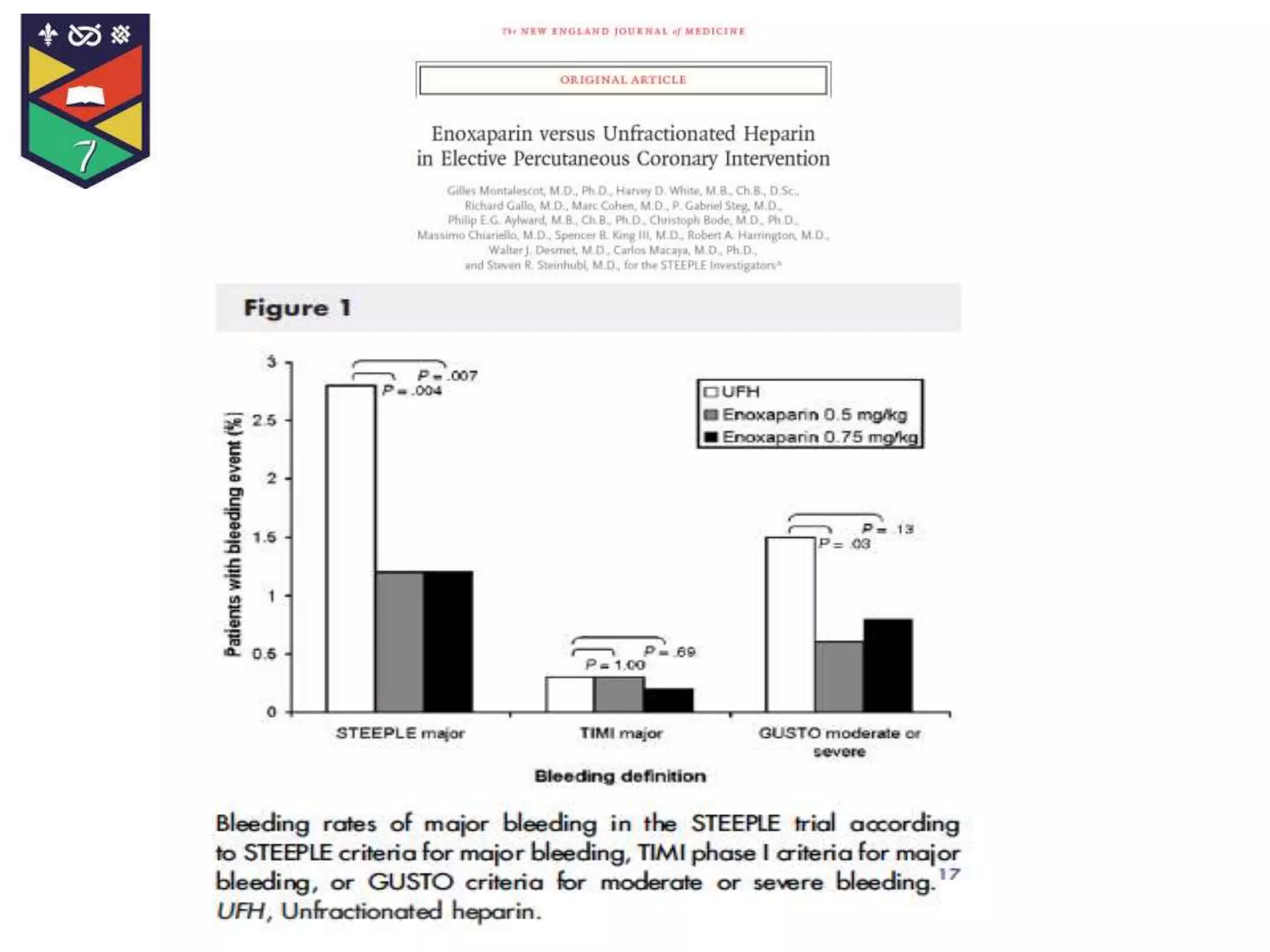
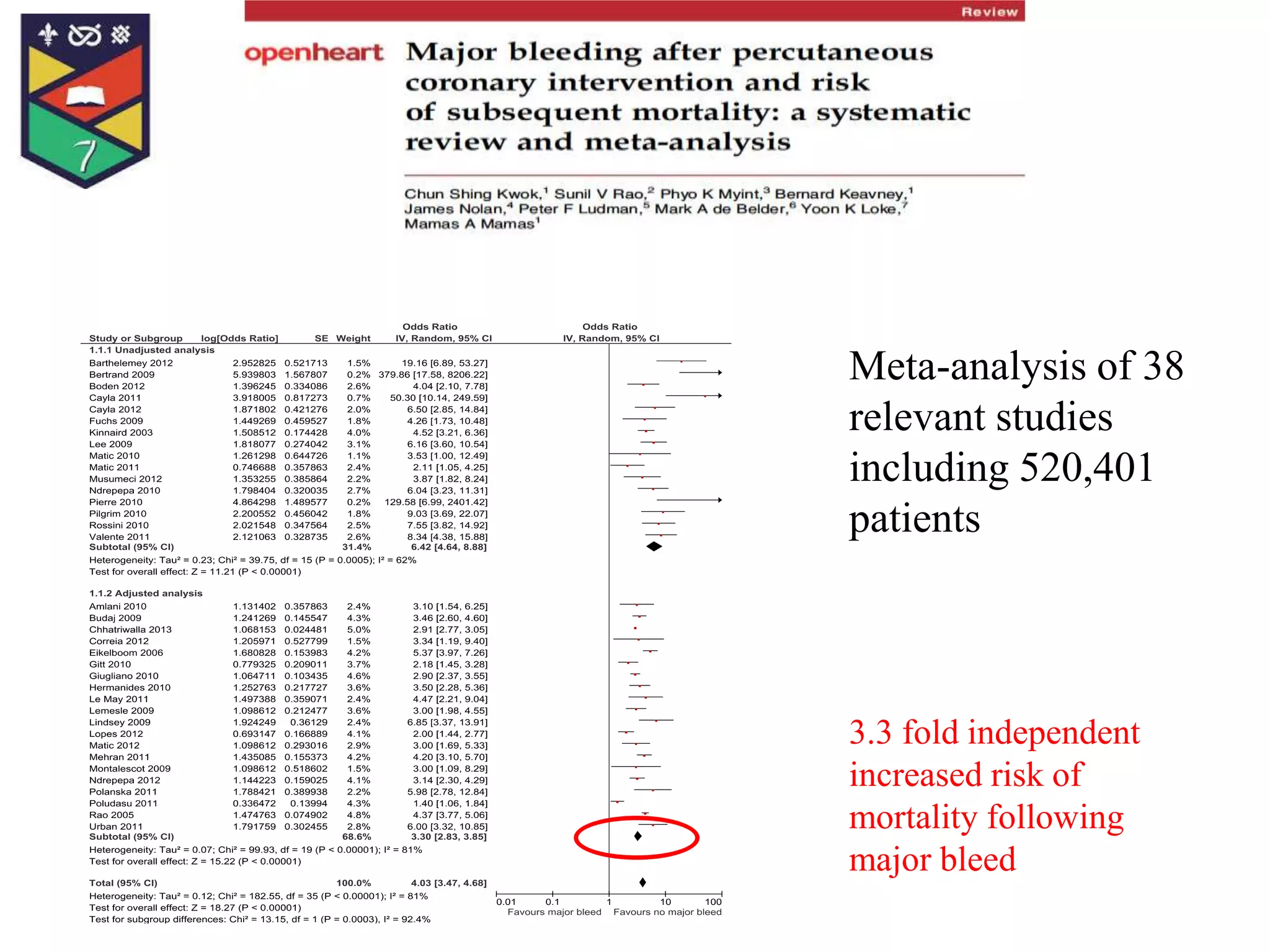
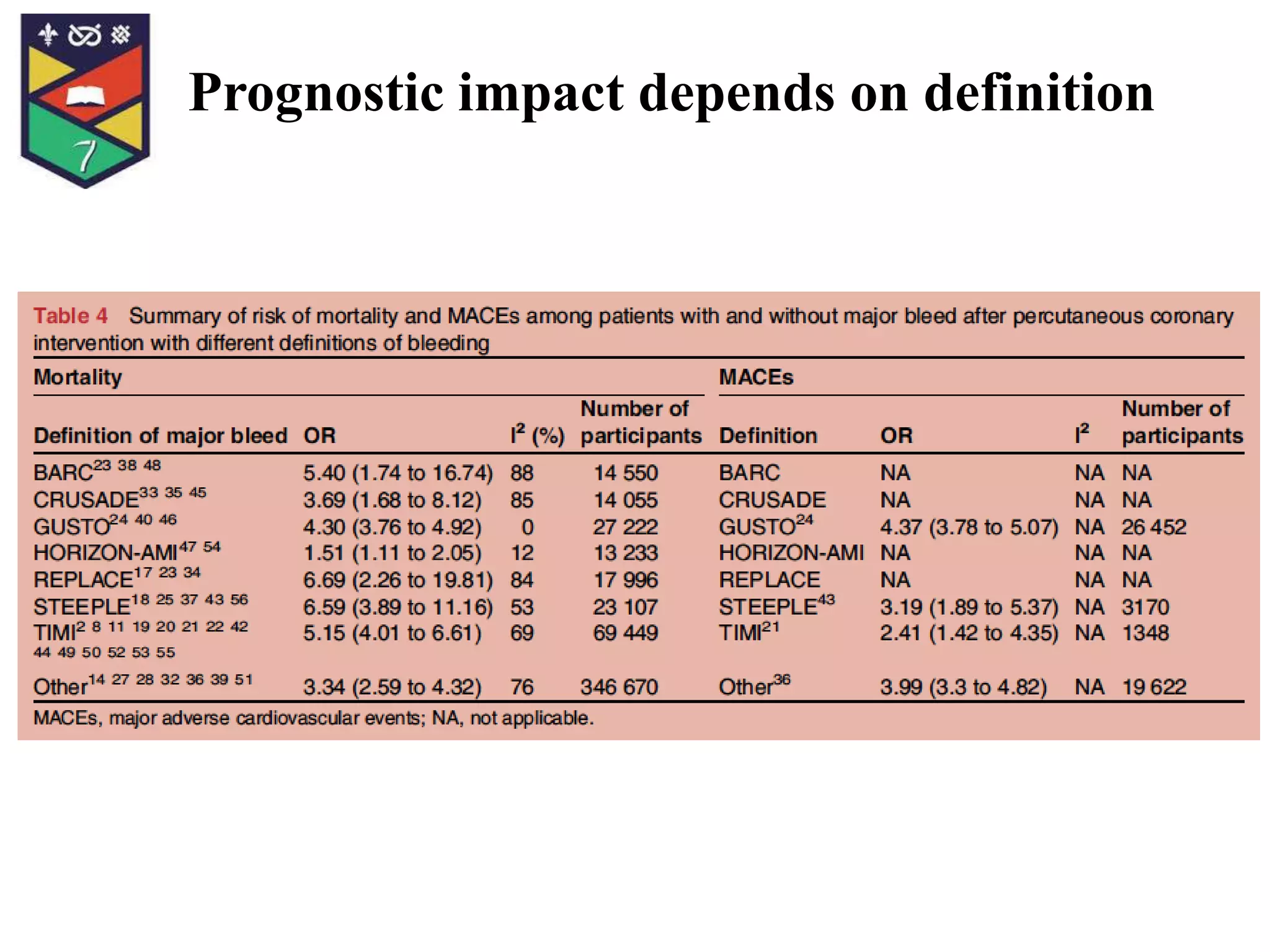
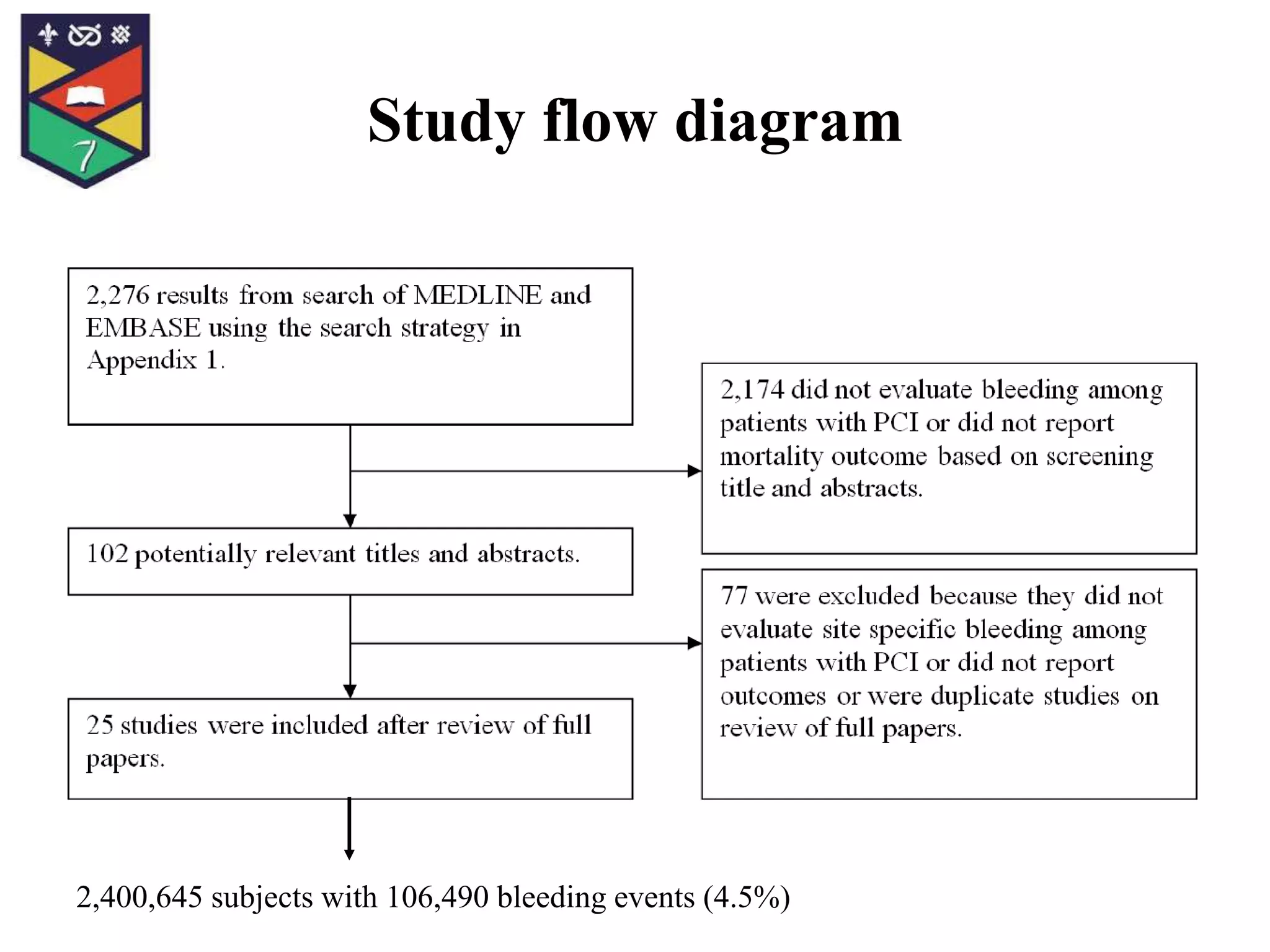
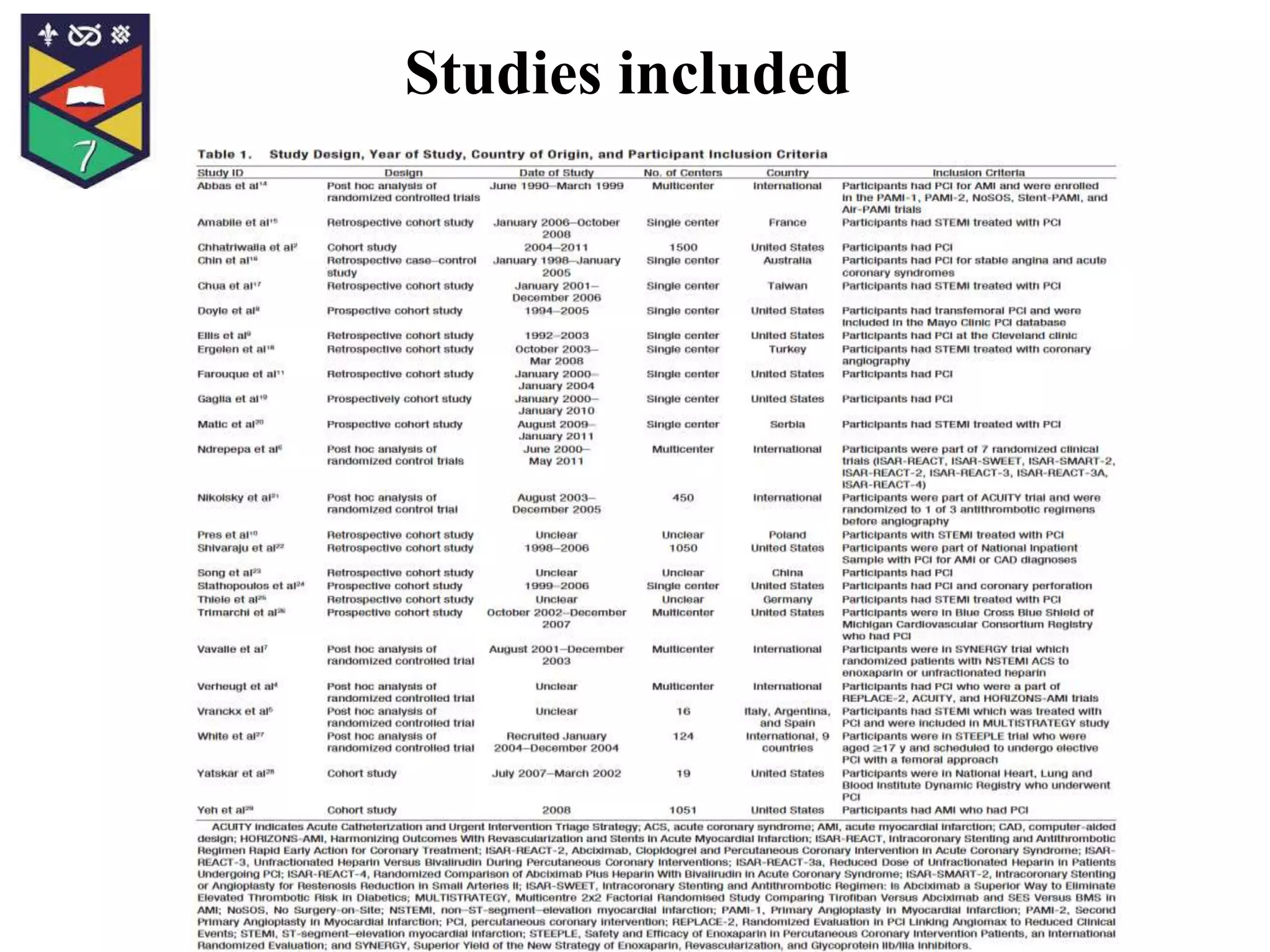
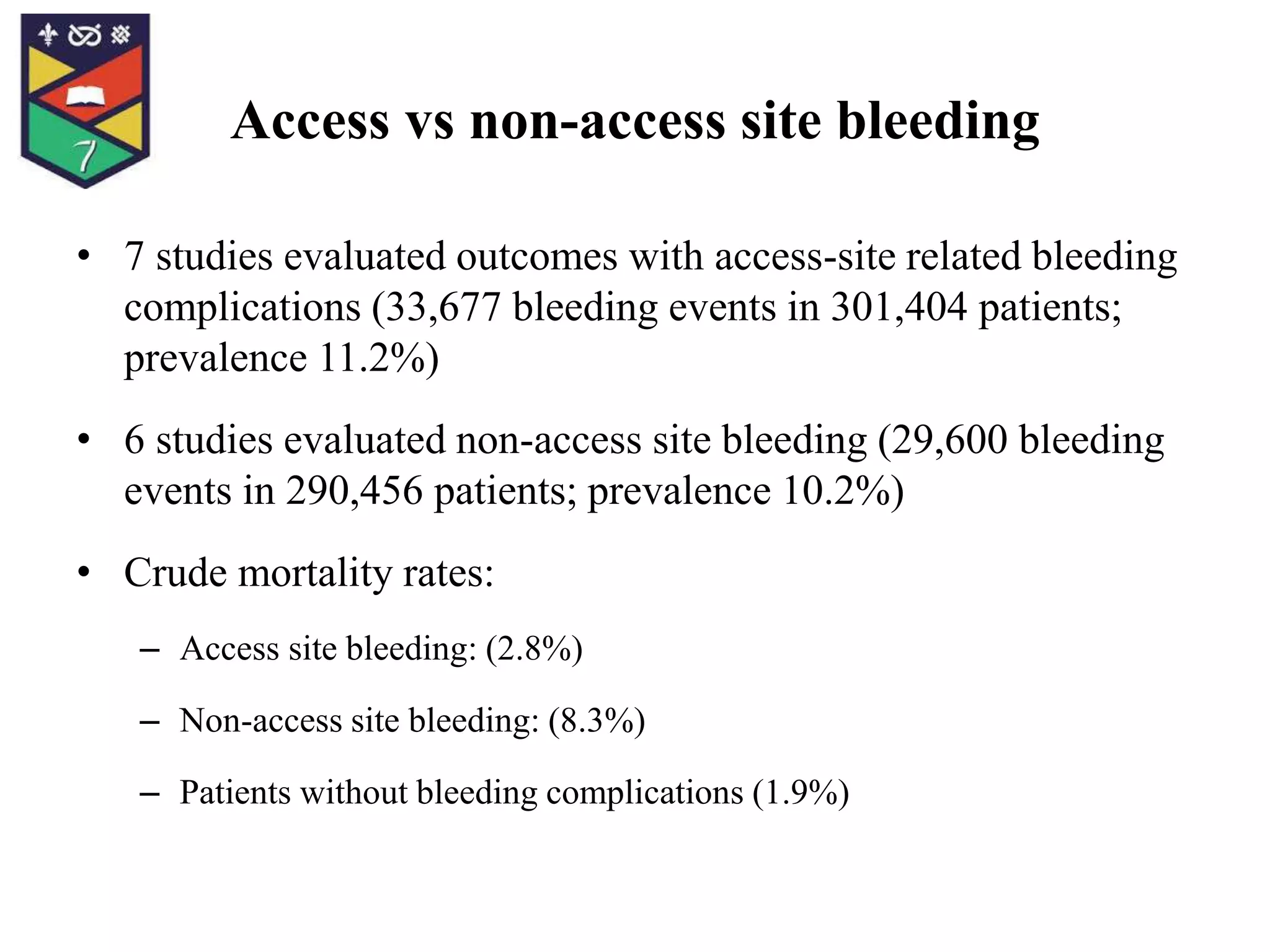
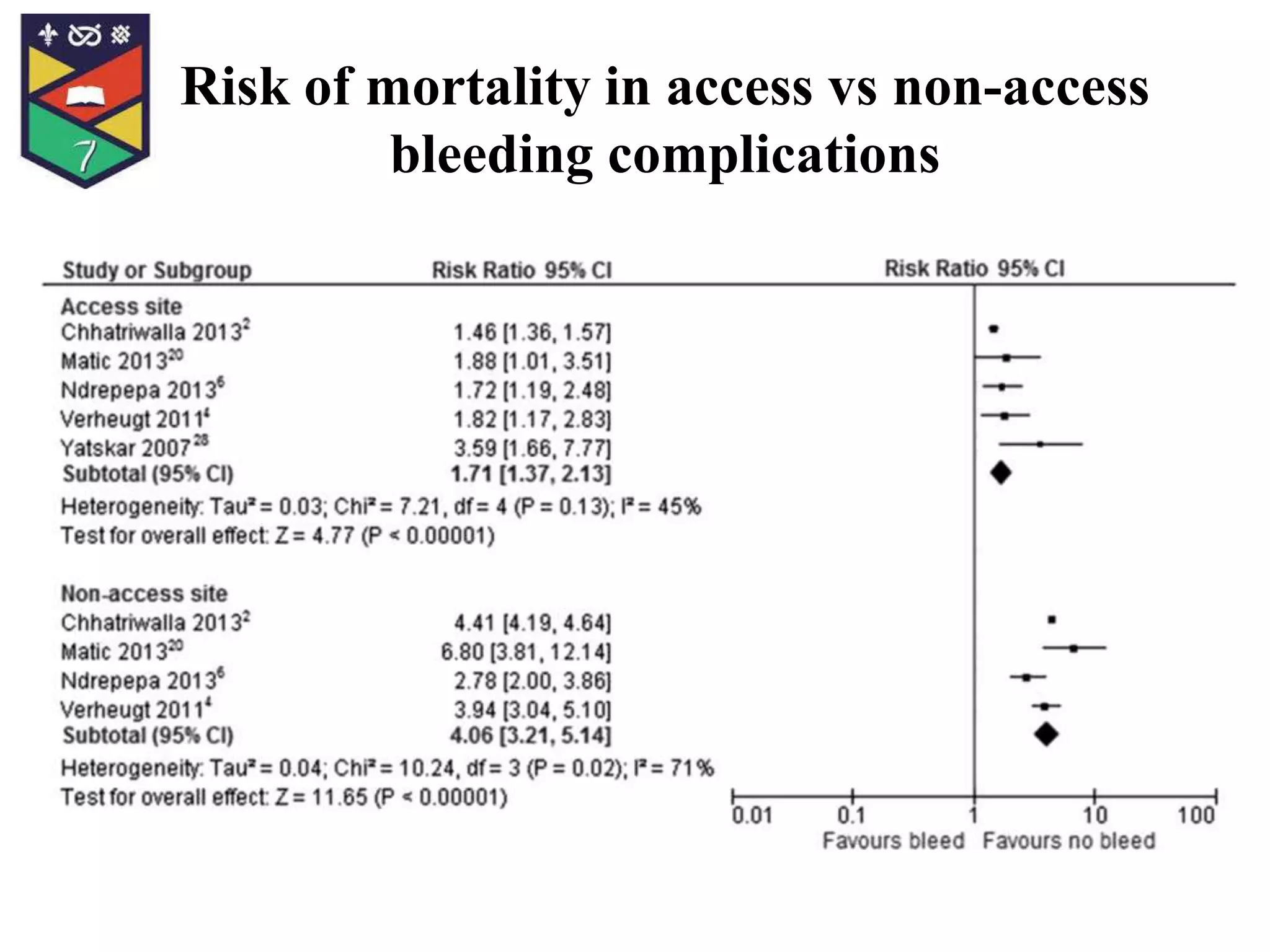
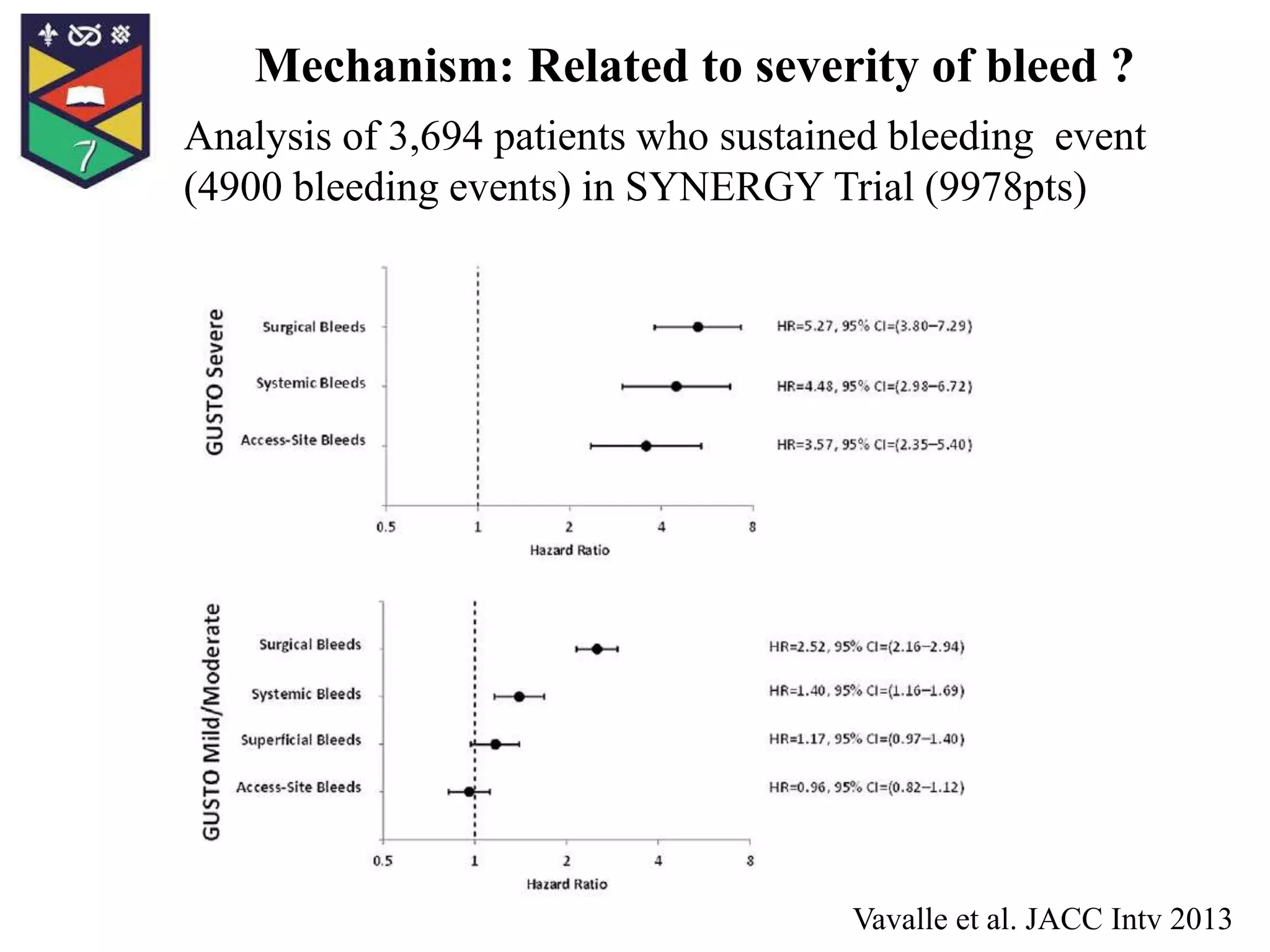
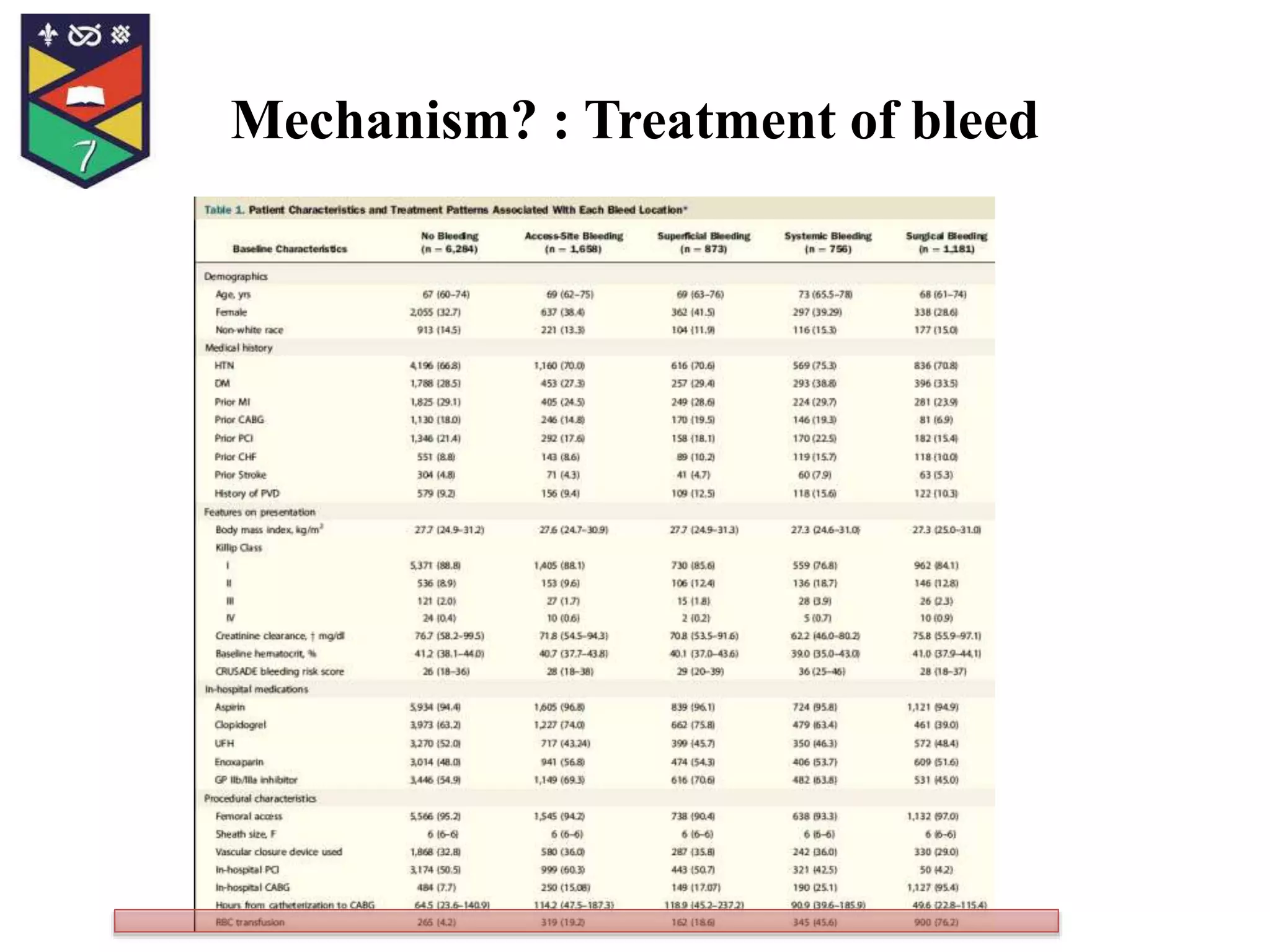
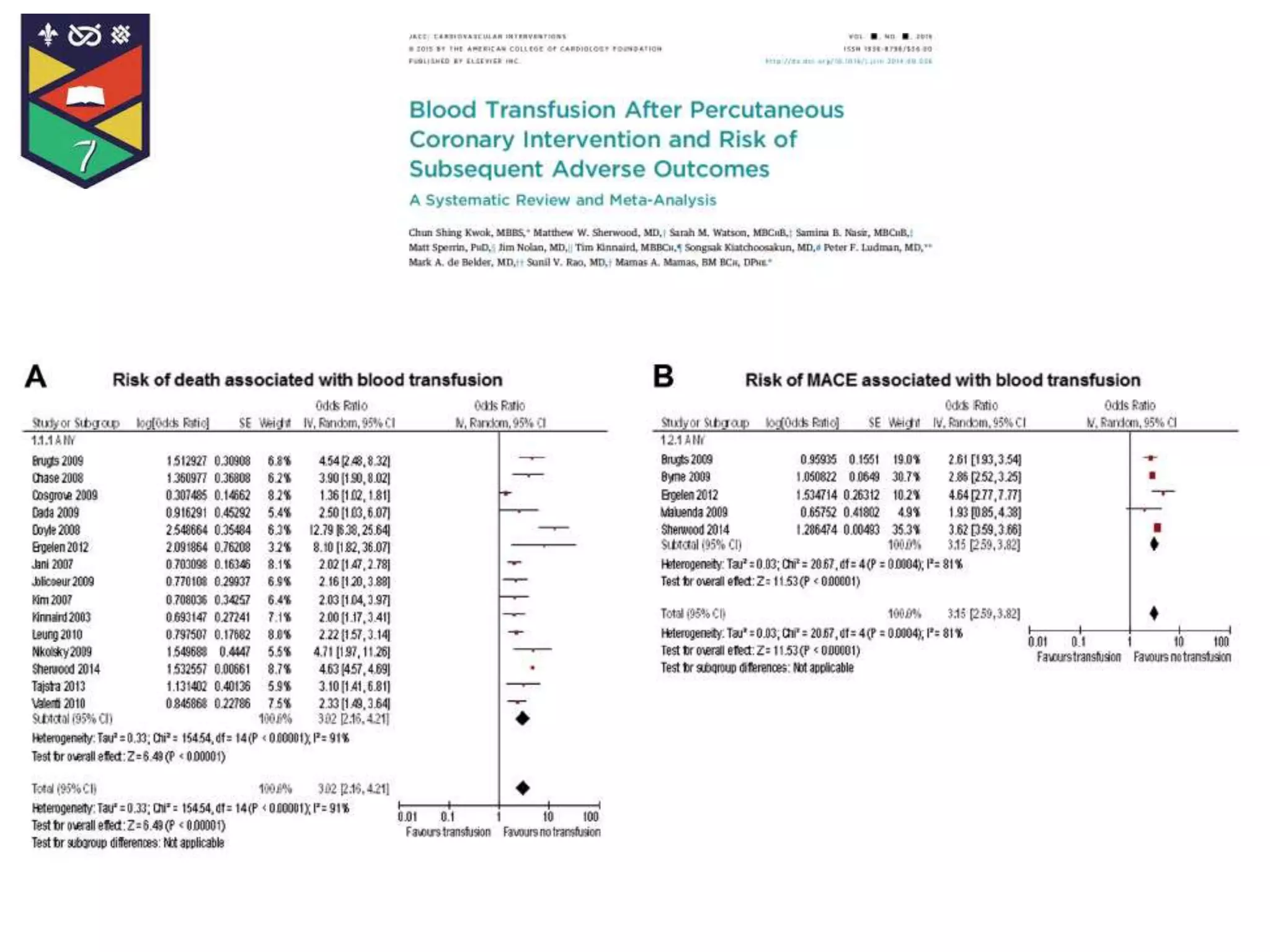
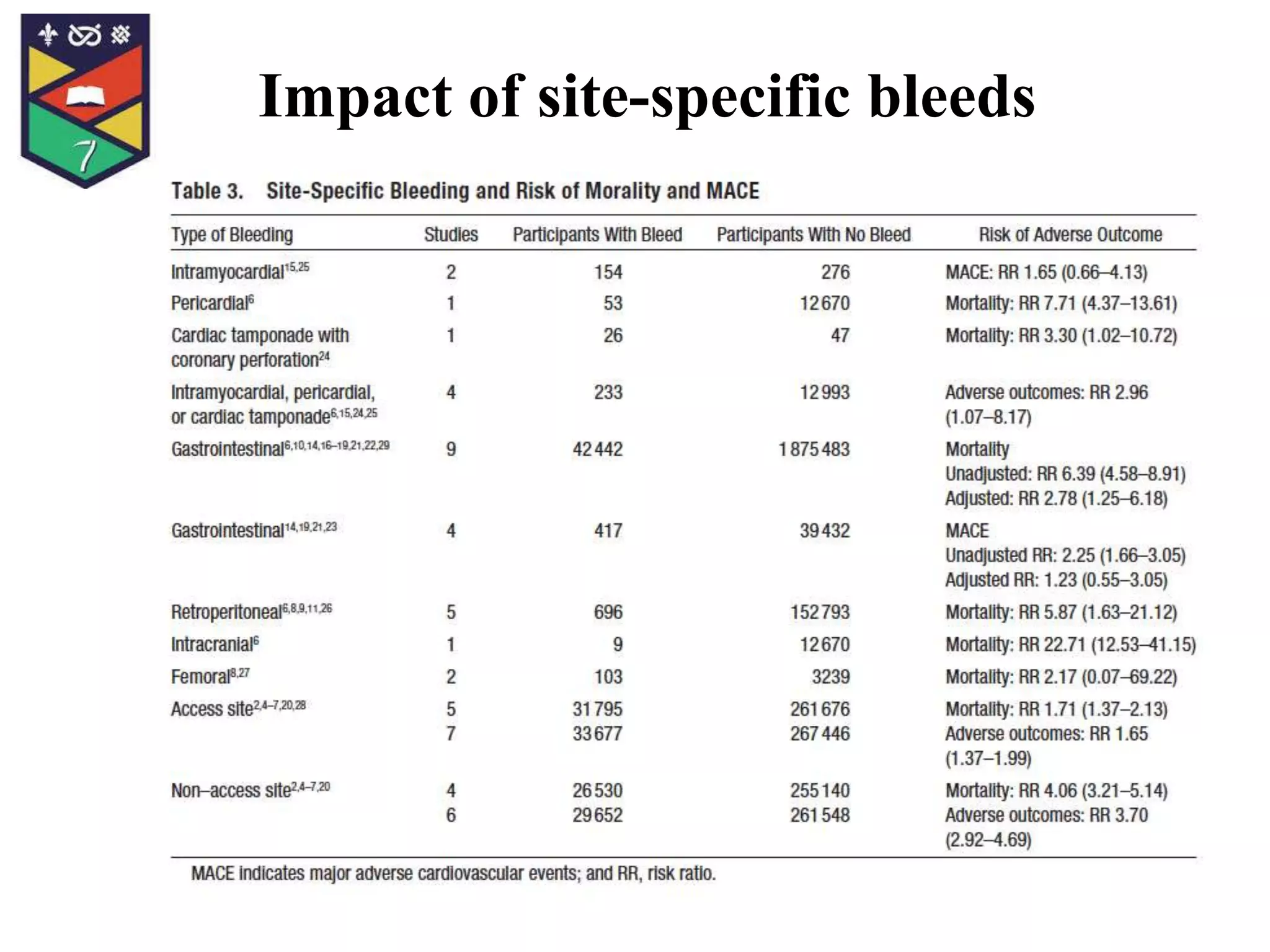
Access vs non-access site bleeding and risk of subsequent mortality and MACE This study aimed to analyze the incidence and prognostic impact of access site versus non-access site bleeding in patients undergoing percutaneous coronary intervention (PCI). The meta-analysis included 38 studies and over 520,000 patients. It found that access site bleeding occurred in 11.2% of patients while non-access site bleeding occurred in 10.2% of patients. However, non-access site bleeding was associated with a higher crude mortality rate of 8.3% compared to 2.8% for access site bleeding. Further analyses confirmed that non-access site bleeding carried a greater risk of subsequent mortality and major adverse cardiac events than access site bleeding. The