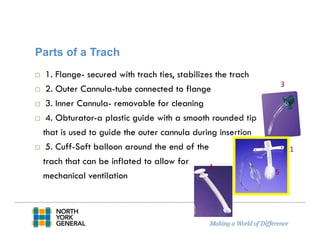
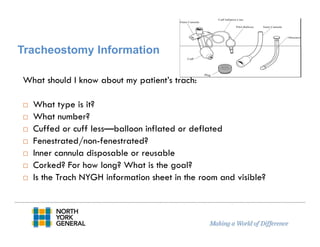
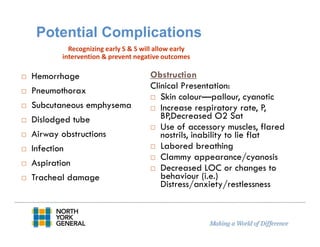
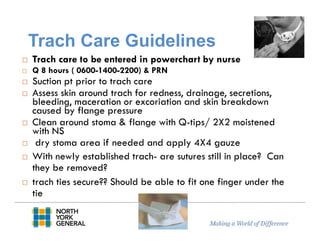
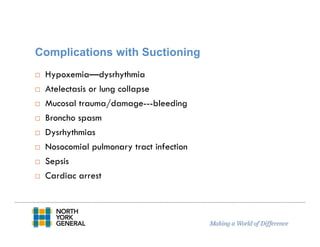
This document reviews guidelines for tracheostomy care and management at NYGH. It defines tracheostomies and the different types. Potential complications are discussed as well as nursing care guidelines including assessment, suctioning, dressing changes, and documentation. Emergency scenarios are also addressed. Tracheostomy care aims to maintain a patent airway and prevent complications through skilled nursing interventions.