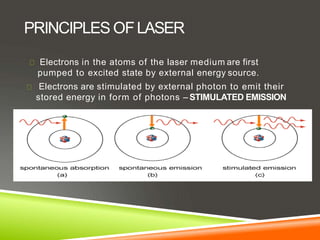
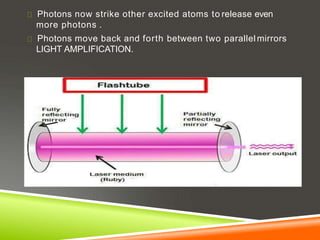
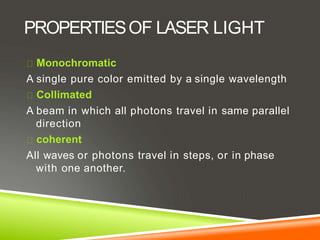
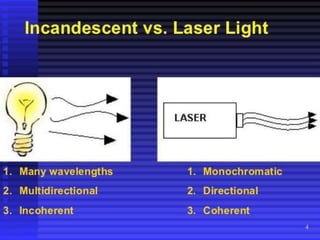
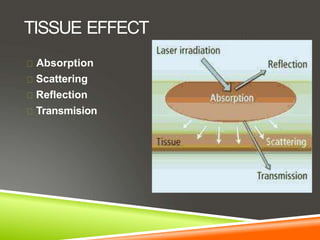
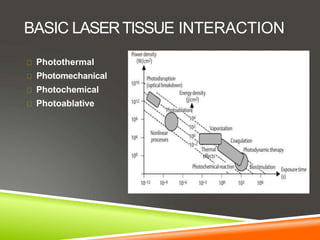
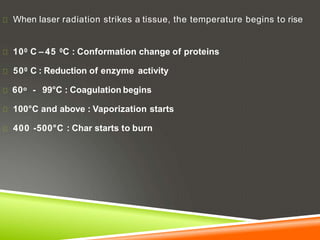
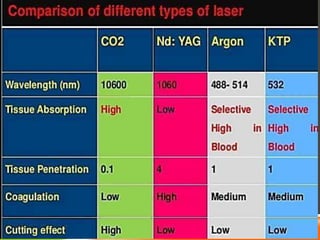
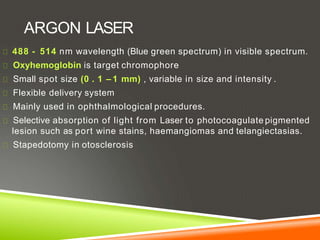
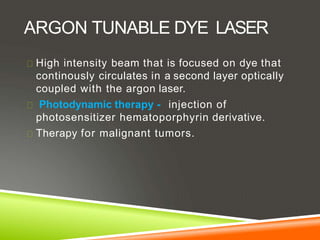
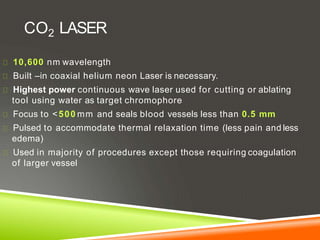
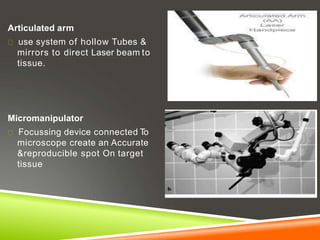
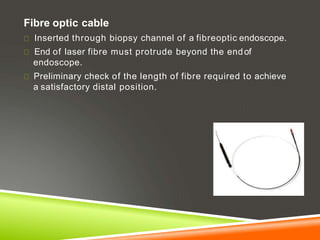
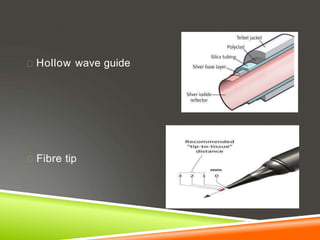
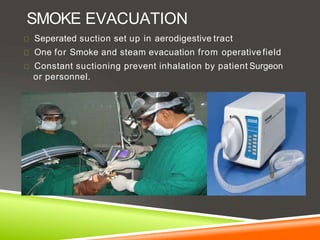
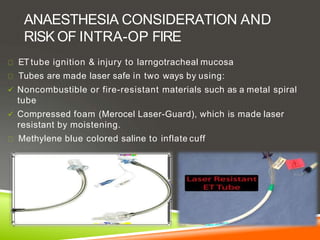
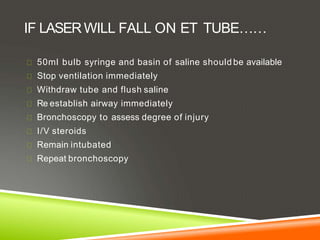
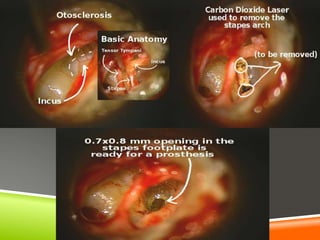
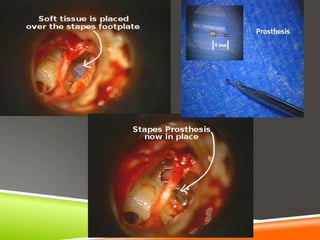
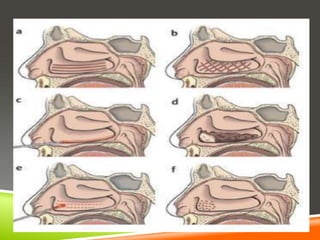
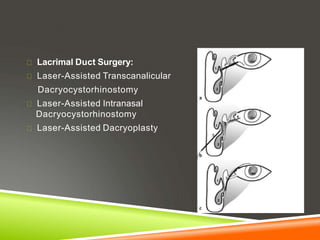
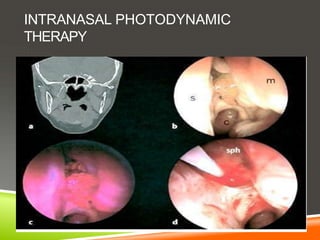
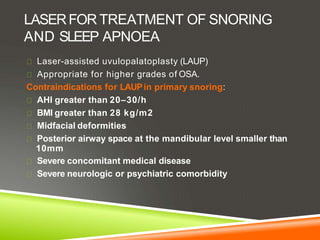
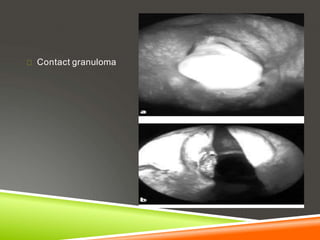
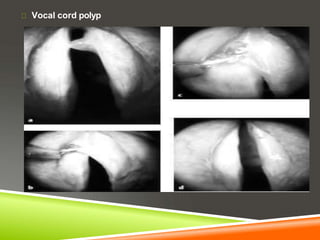
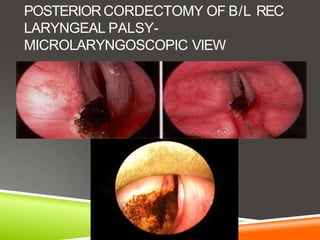
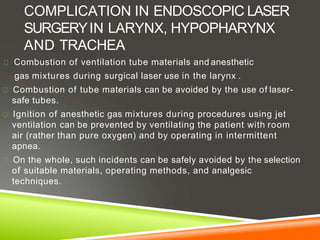
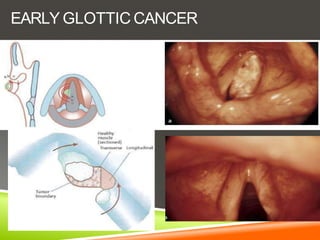
The document discusses the use of lasers in otolaryngology. It begins with an introduction to lasers and their principles. It then describes different types of lasers used including CO2, Nd:YAG, KTP, argon lasers and their properties. Applications of lasers in ENT are discussed including uses in otology like stapes surgery, external auditory canal procedures and middle ear surgery. Rhinology procedures like turbinate reduction and septal surgery are also covered. Uses of lasers in oral cavity, pharynx, larynx and neck are summarized. Safety considerations with lasers and their delivery systems are provided.