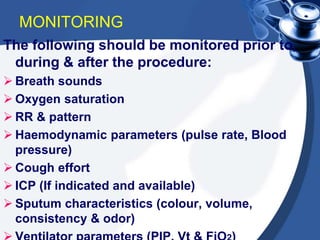
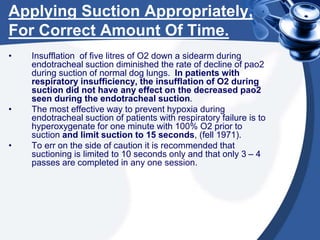
This document provides guidance on suctioning techniques for nursing students. It aims to teach safe and effective use of suction equipment. The objectives are to familiarize students with anatomy related to suctioning and how to properly set up equipment, identify the need for suctioning, and demonstrate techniques while minimizing trauma. The document covers the definition of suctioning, its history, related anatomy, purposes, guidelines, types of suctioning, monitoring, choosing the correct catheter size and suction pressure, applying suction for the appropriate time, and assessing outcomes. Contraindications and limitations are also discussed.