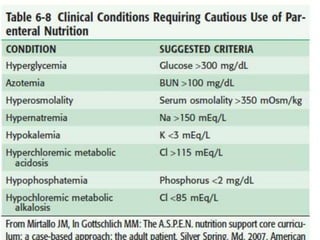
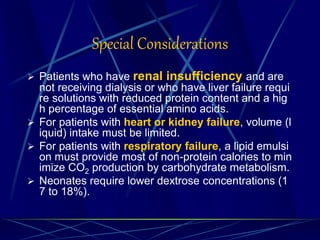
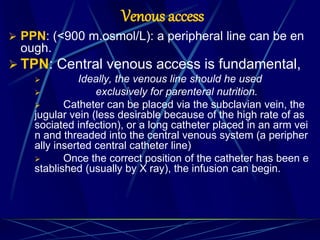
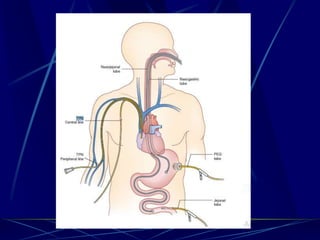
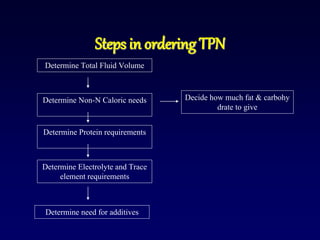
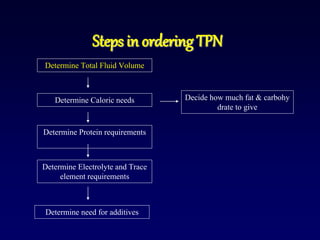
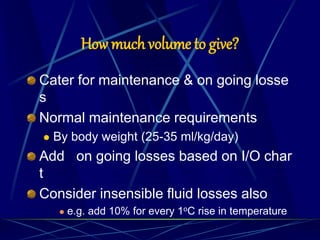
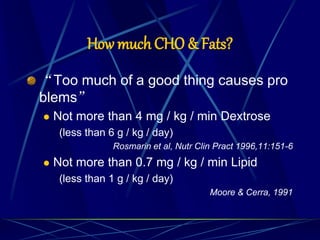
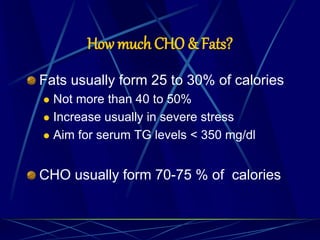
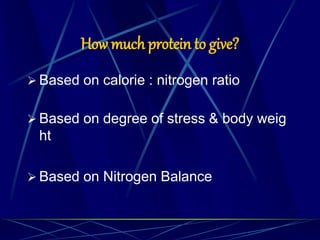
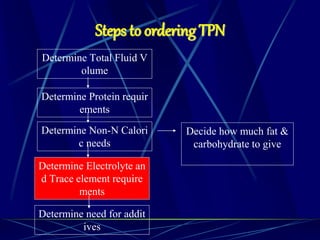
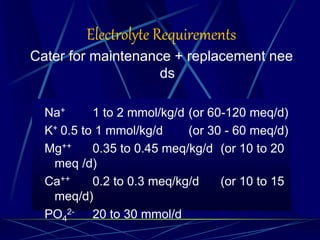
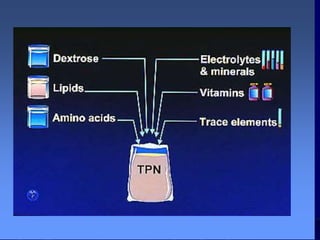
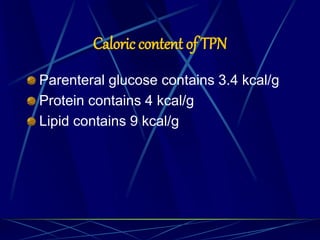
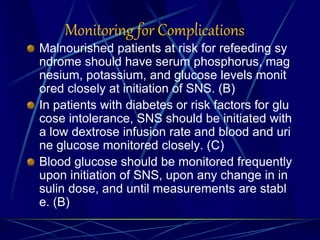
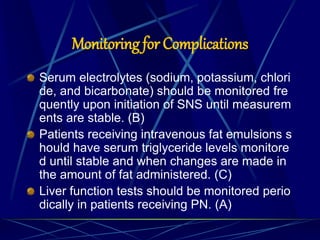
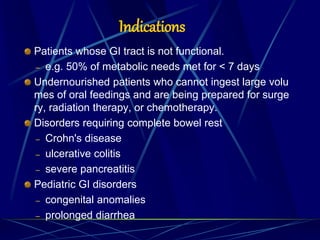
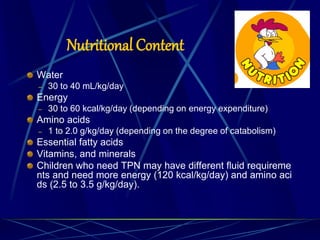
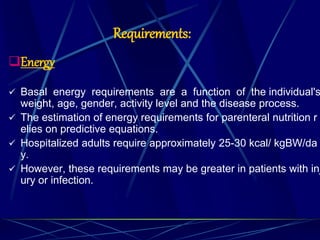
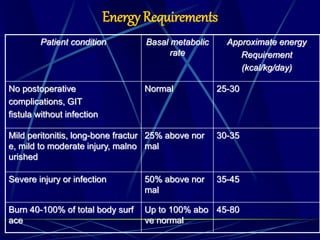
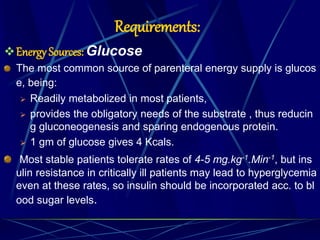
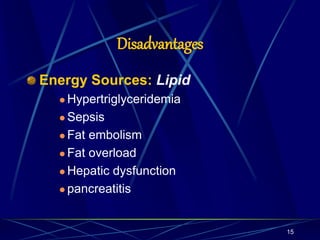
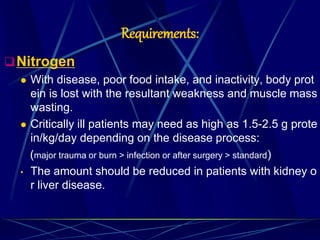
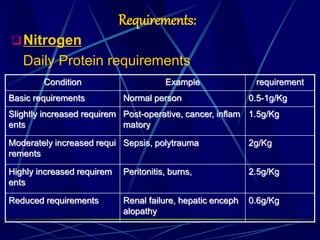
Total parenteral nutrition (TPN) involves supplying nutrients intravenously. TPN may be used when the gastrointestinal tract is not functional, such as for patients who cannot meet at least 50% of their metabolic needs for over 7 days or undernourished patients preparing for surgery. The goals of TPN are to decrease catabolism, support metabolism, and improve organ function. TPN solutions provide water, energy from glucose and lipids, amino acids for protein, electrolytes, vitamins, and minerals tailored to individual patient needs. Careful monitoring is required due to risks such as hyperglycemia, hypertriglyceridemia, and infections.
![Anthropometry
• Weight for Height comparison
• Body Mass Index [BMI <19]
• Triceps-skinfold (index of body fat)
• Mid arm muscle circumference(muscle mass)
• Bioelectric impedance
• Hand grip dynamometry
• Clinical Assessment score(SGA)
score of history and clinical examination
Nutritional Assessment](https://image.slidesharecdn.com/tpn1-160119100131/85/Total-parental-nutrition-36-320.jpg)