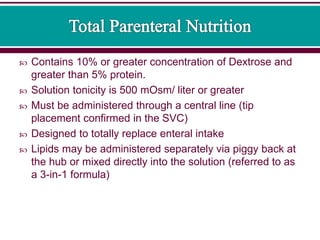
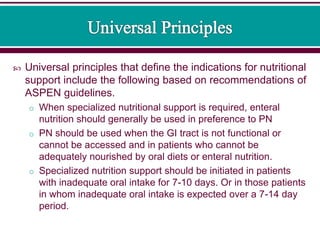
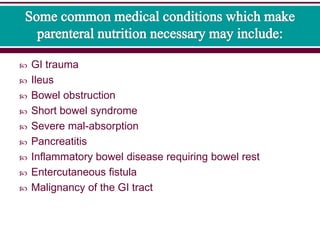
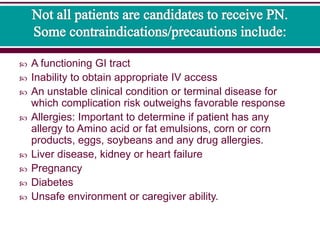
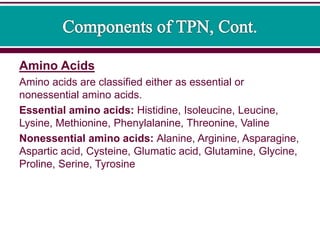
Parenteral nutrition (PN) involves administering nutrients intravenously and is considered when a patient is unable to meet nutritional needs enterally. PN can be partial (PPN), containing less than 10% dextrose, or total (TPN), containing greater amounts. PN provides proteins, carbohydrates, lipids, vitamins, minerals, electrolytes and water to meet nutritional needs. Close monitoring is required to prevent deficiencies or complications from excess levels.