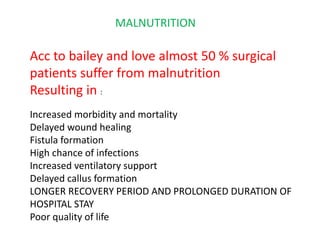
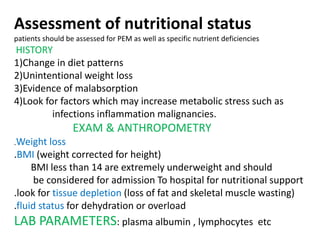
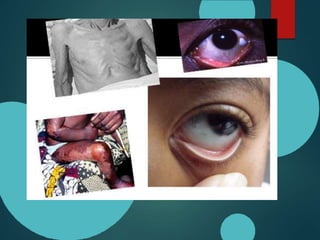
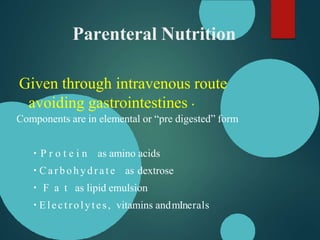
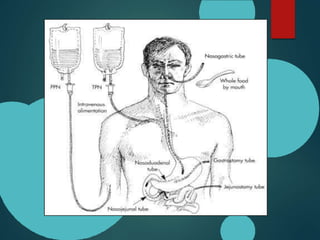
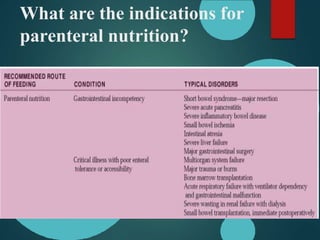
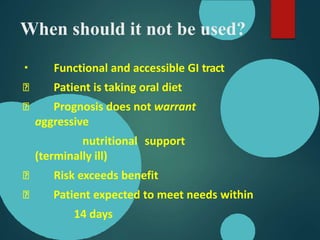
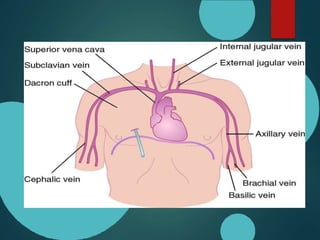
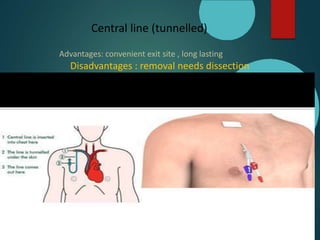
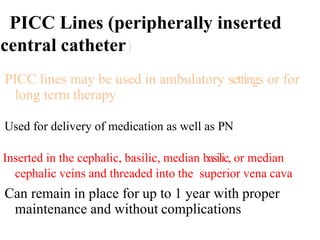
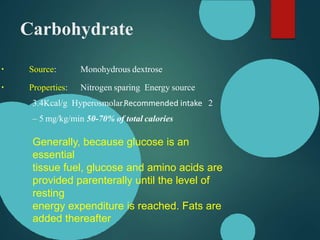
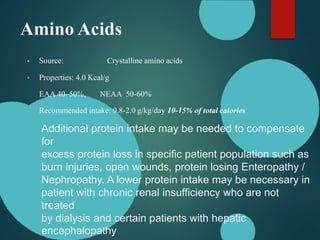
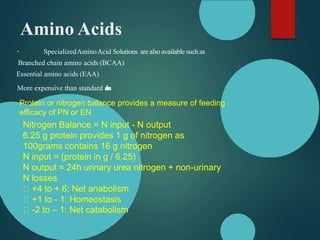
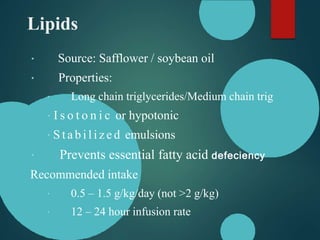
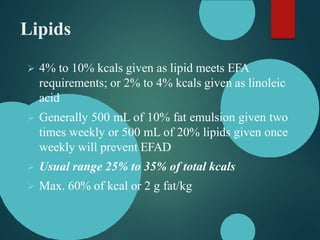
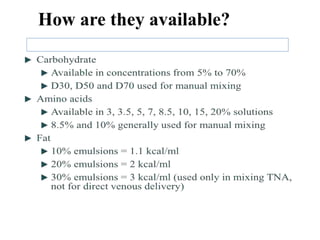
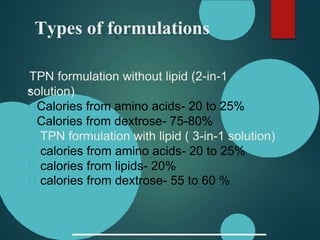
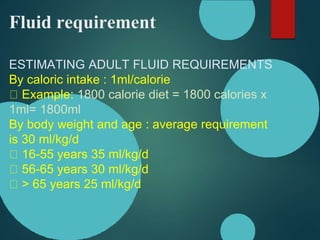
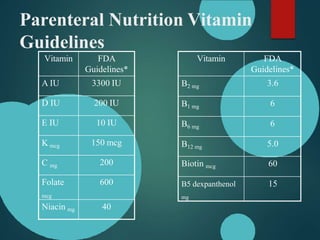
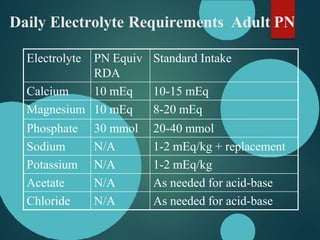
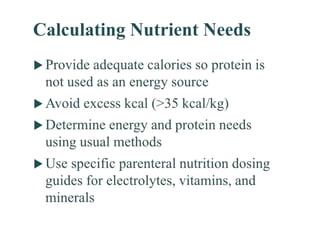
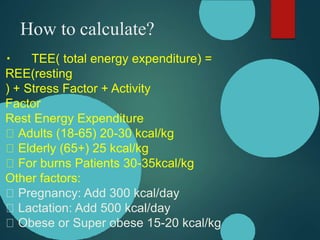
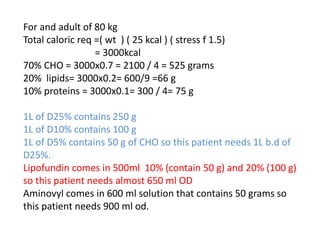
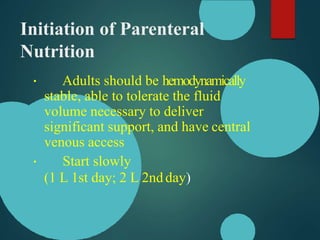
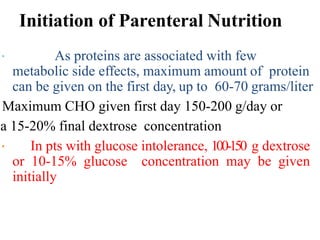
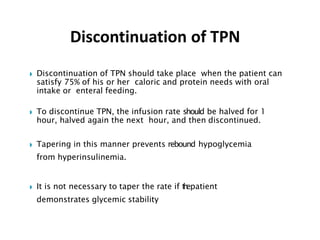
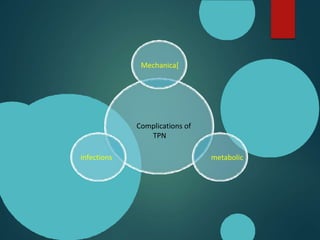
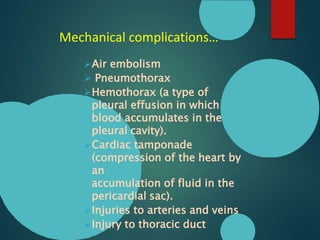
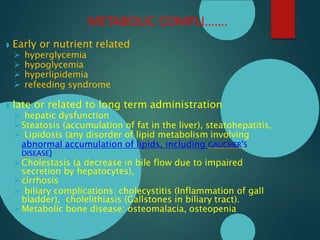
This document discusses total parenteral nutrition (TPN). It begins by outlining the indications for TPN, including malnutrition and inability to meet nutritional needs enterally. The document then covers the components of TPN including carbohydrates, amino acids, lipids, electrolytes, vitamins and minerals. It discusses the methods of administering TPN including peripherally and through central lines. The document provides guidance on calculating nutritional requirements and initiating and monitoring TPN. Finally, it reviews potential complications of TPN including mechanical issues, metabolic disturbances, and infections.