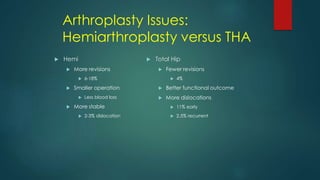
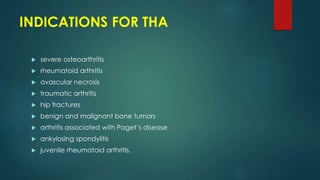
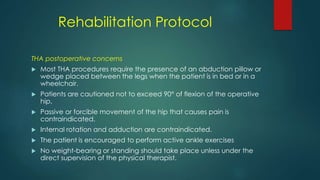
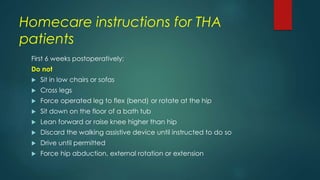
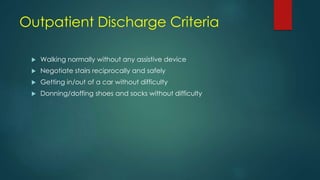
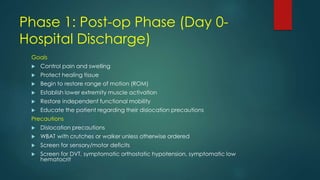
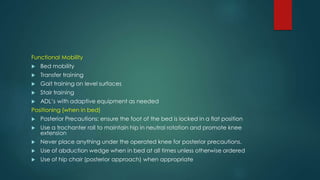
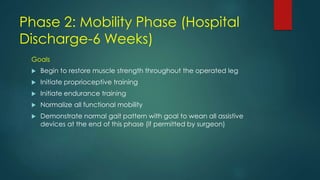
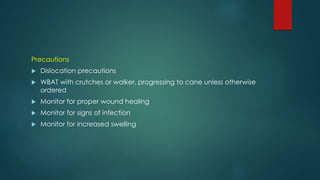
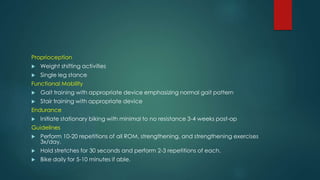
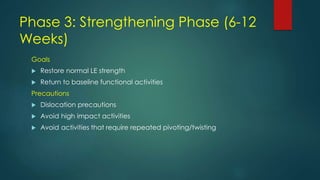
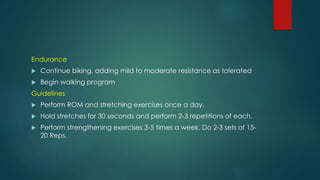
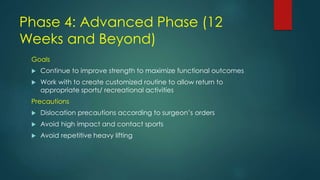
Hip fractures in the elderly can be life-altering and lead to high mortality rates. Total hip arthroplasty (THA) is commonly used to treat hip fractures and arthritis, involving replacing damaged bone and cartilage with prosthetic components. Post-operative rehabilitation focuses on restoring range of motion and strength over 4 phases, while avoiding activities that could dislocate the hip.