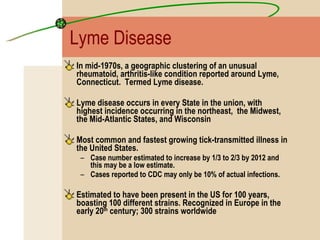
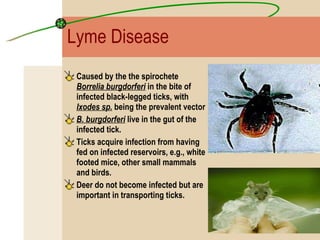
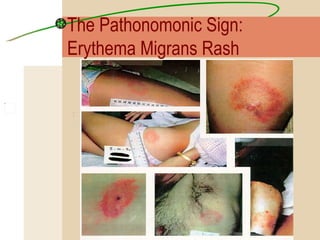
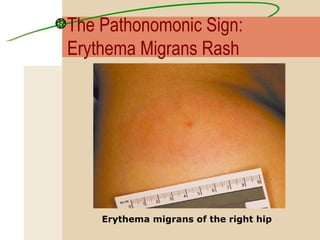
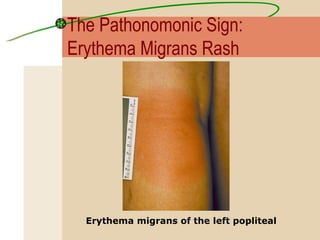
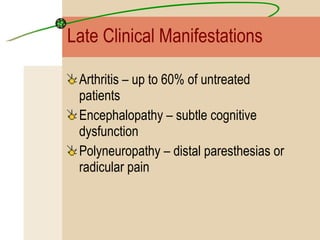
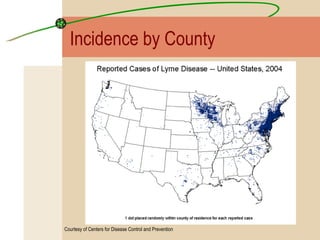
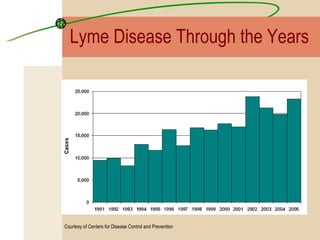
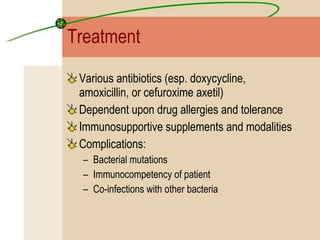
Lyme disease is caused by the bacterium Borrelia burgdorferi transmitted through the bite of infected blacklegged ticks. It was first reported in Lyme, Connecticut in the 1970s. Symptoms vary depending on the stage of infection and can include an expanding skin rash, joint pain, and neurological issues. While most cases can be treated with antibiotics, prevention through protective clothing and tick checks is important. Ongoing research is exploring how environmental factors like acorn crops influence tick and mouse populations in transmitting the disease.