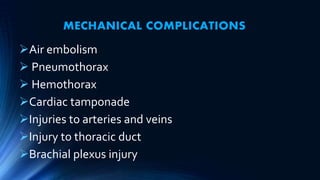
Parenteral nutrition (PN) can result in numerous complications if not carefully monitored. Mechanical complications include injuries from catheters. Metabolic complications involve issues like hyperglycemia, hepatic dysfunction, and refeeding syndrome. Infections from catheters are also common. Close monitoring of patients on PN is necessary to check for metabolic and clinical issues and manage complications. Careful attention to nutrient levels and other medical factors can help reduce risks.