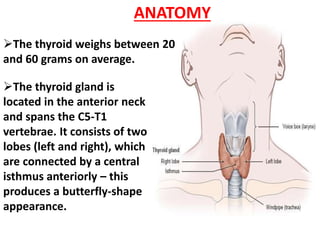
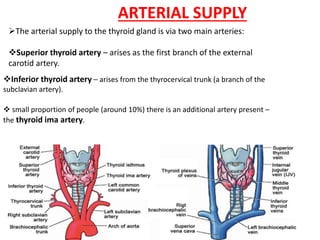
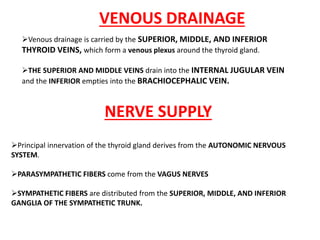
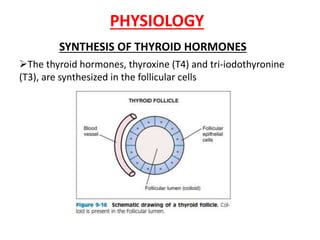
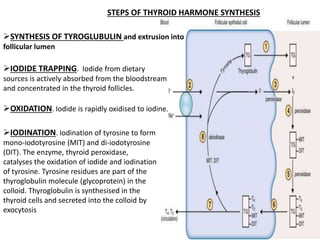
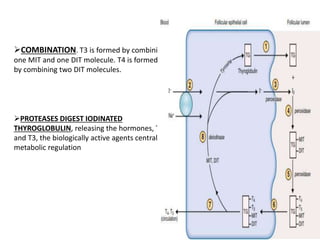
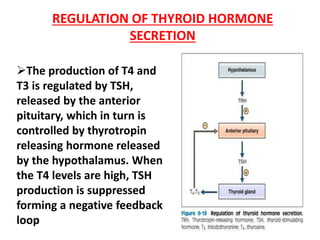
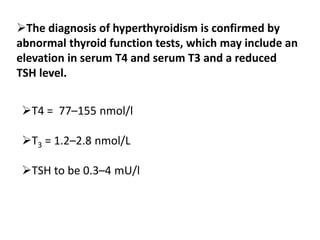
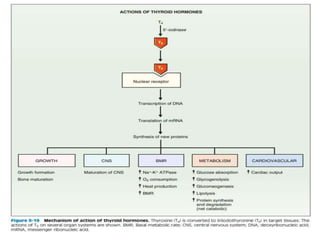
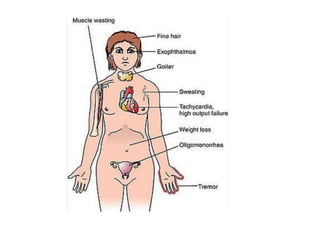
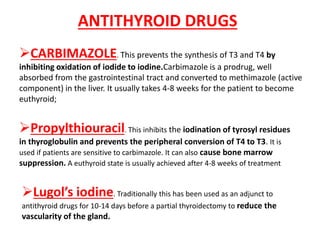
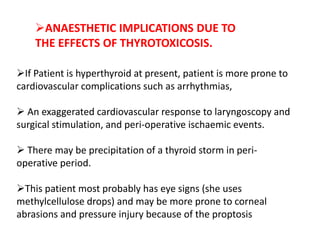
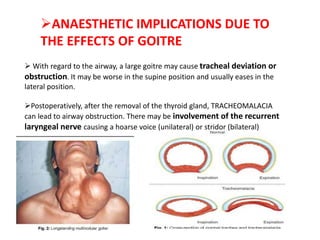
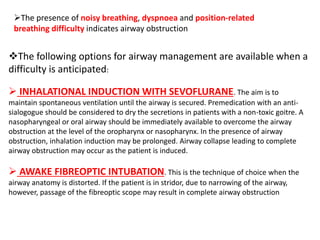
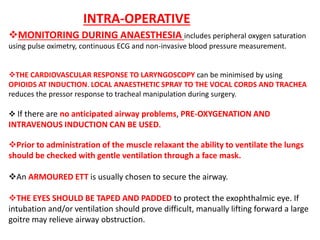
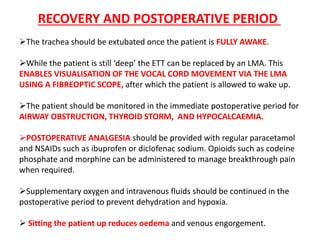
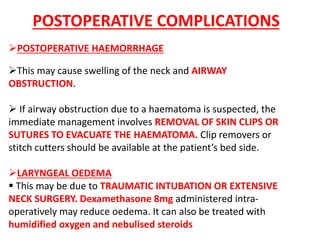
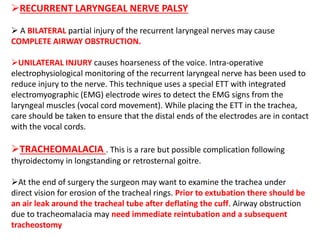
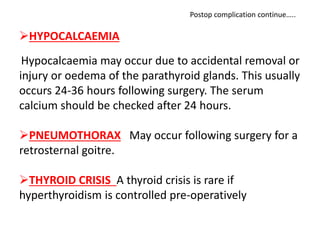
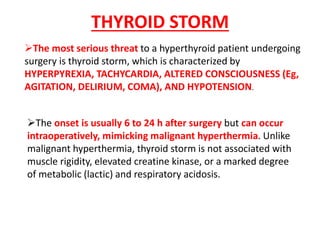
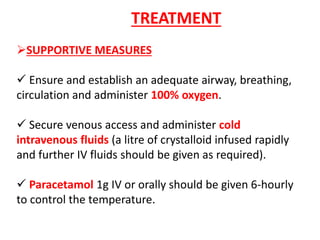
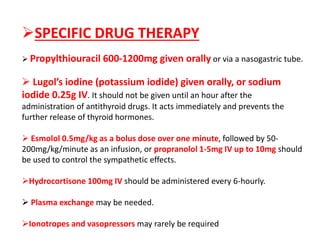
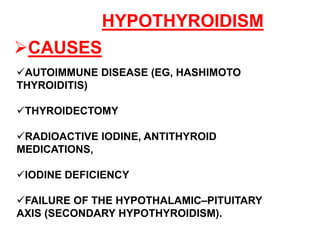
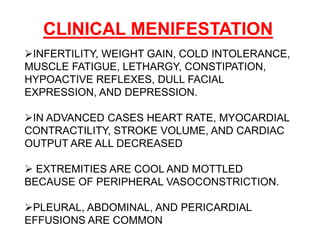
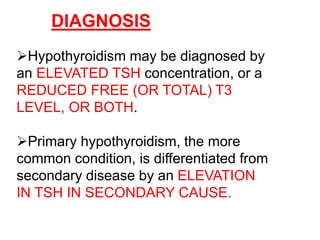
The document discusses the anatomy, physiology, and clinical management of the thyroid gland and hyperthyroidism. It describes the thyroid's location in the neck, its blood supply, hormone production, and regulation. It then covers the signs and causes of hyperthyroidism, investigations, medical management using antithyroid drugs, and anaesthetic implications for thyroidectomy. Postoperative complications like hemorrhage and laryngeal edema are also mentioned.