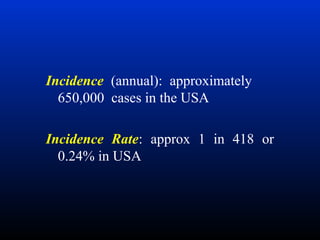
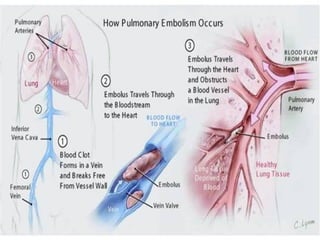
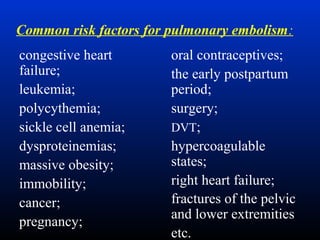
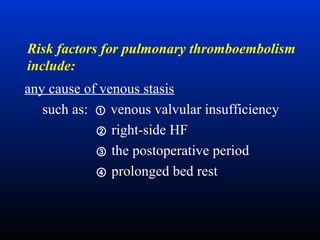
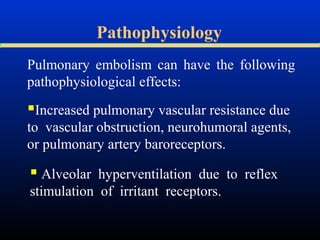
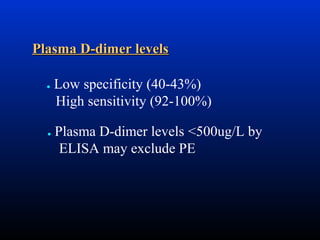
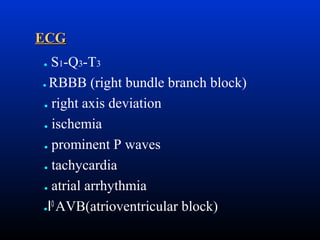
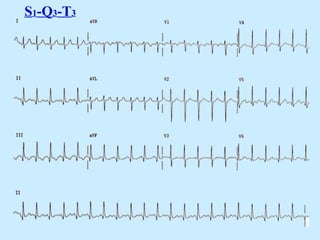
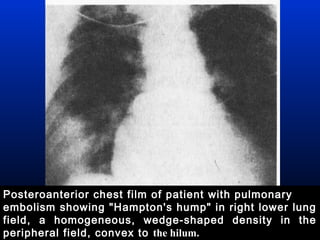
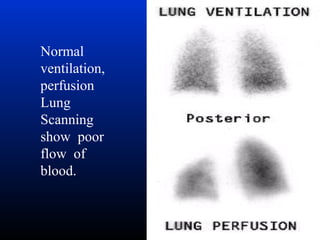
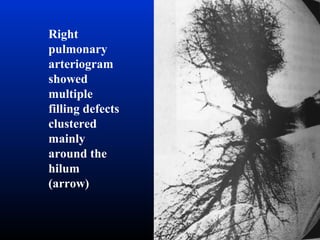
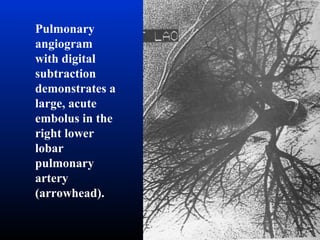
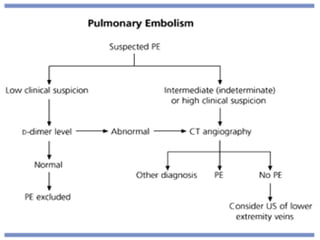
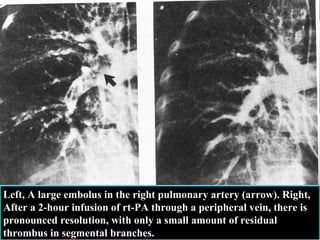
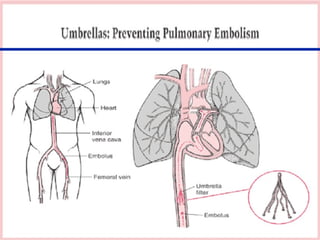
This document discusses different types of thromboembolism including pulmonary embolism, fat embolism, air embolism, and amniotic fluid embolism. It provides details on the definition, causes, risk factors, symptoms, diagnosis, treatment and prognosis of pulmonary embolism, which is the most common type of thromboembolism. The document also discusses the pathophysiology and mechanisms of the different embolism types.