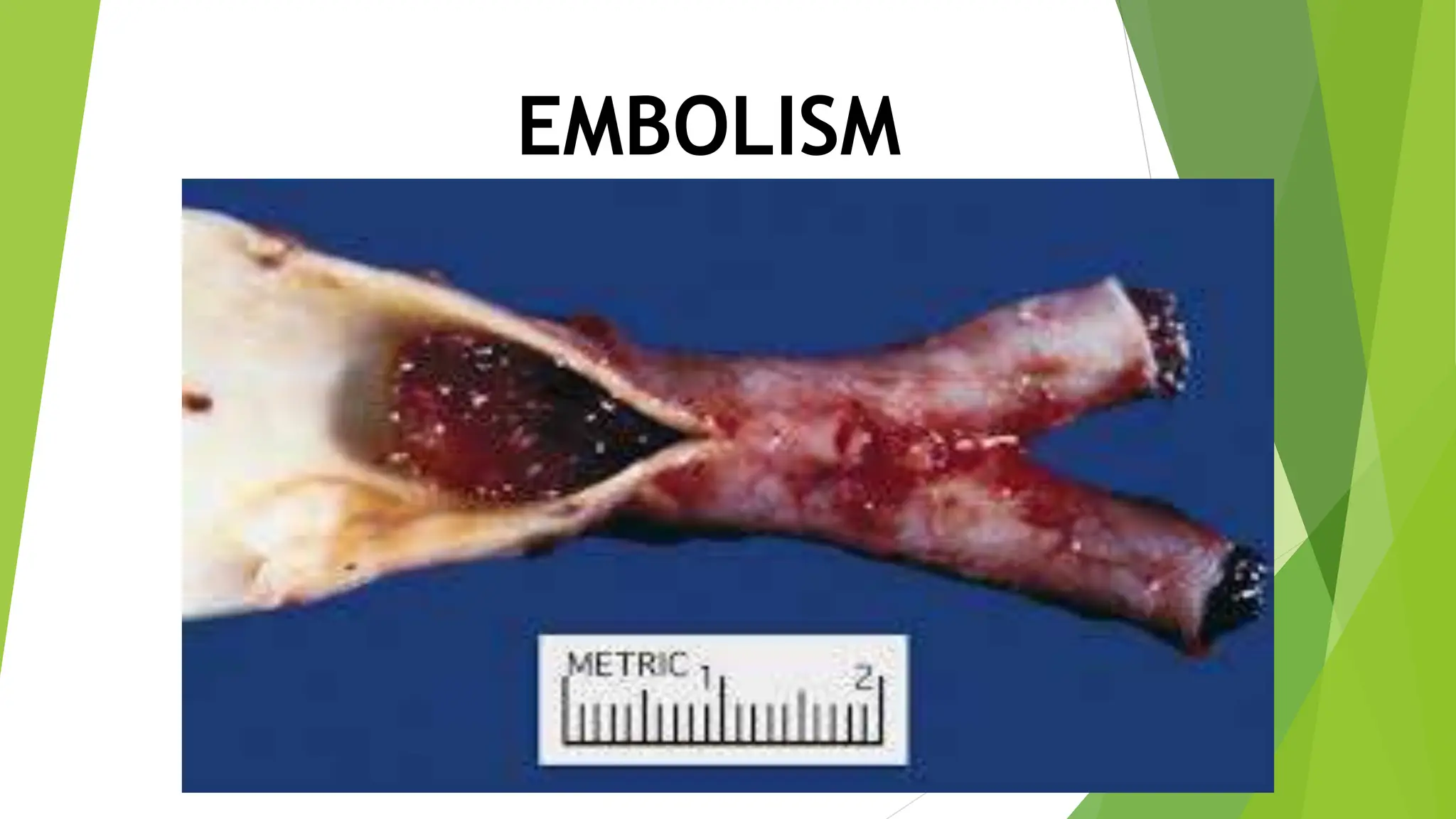
An embolism occurs when a particle or blood clot obstructs blood flow. Common types include pulmonary (lung) and brain embolisms. Pulmonary embolisms are usually caused by blood clots that break off and travel to the lungs from deep veins in the legs. Risk factors include prolonged immobility, recent surgery or injury, smoking, oral contraceptives, and obesity. Symptoms include shortness of breath, chest pain, and coughing up blood. Diagnosis involves blood tests, CT scans, ultrasound, and angiograms. Treatment focuses on anticoagulants and thrombolytic drugs to dissolve clots along with managing pain and oxygen levels.