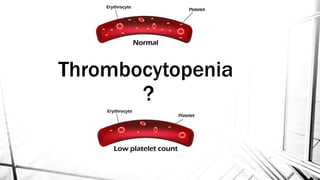
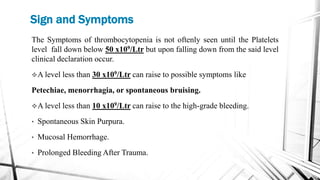
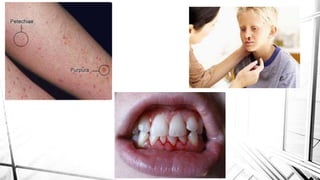
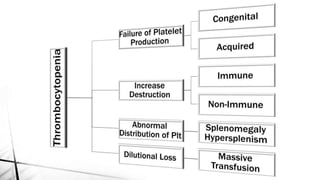
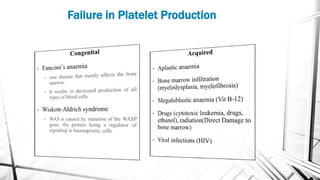
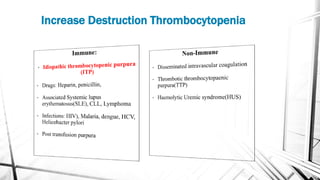
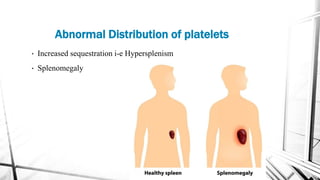
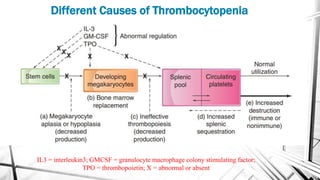
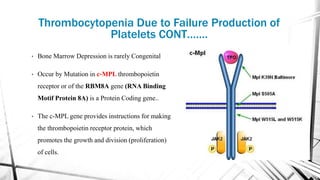
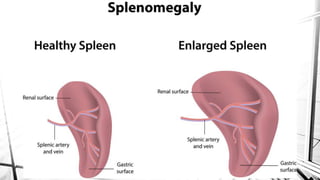
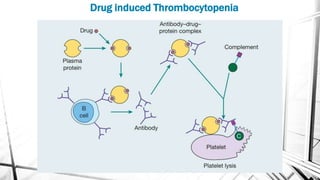
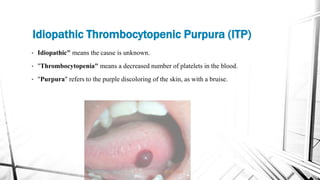
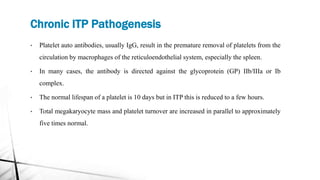
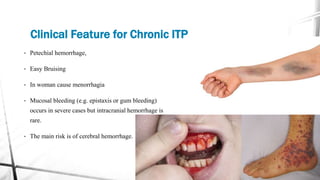
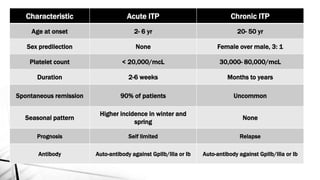
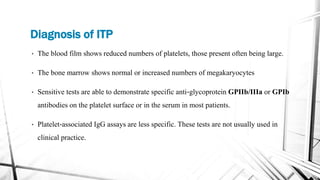
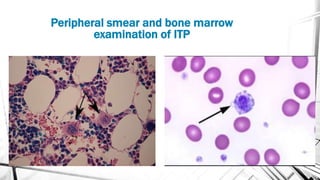
The document discusses thrombocytopenia, characterized by a low platelet count, its causes, diagnosis, and treatment options. It details various types of thrombocytopenia, including idiopathic thrombocytopenic purpura (ITP), and outlines their clinical features, diagnostic procedures, and management strategies. Additionally, case scenarios illustrate potential presentations and diagnoses of thrombocytopenia in patients.