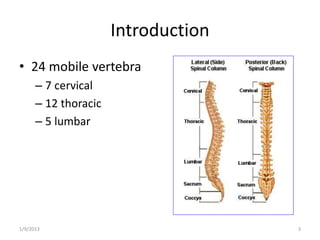
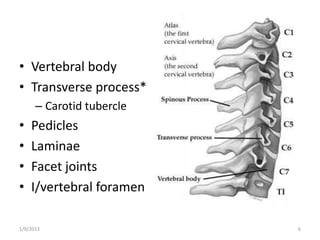
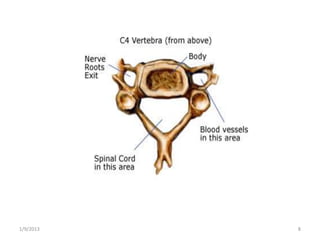
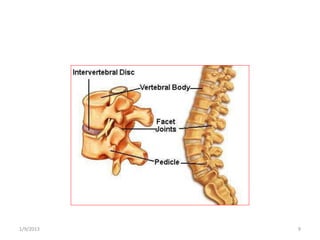
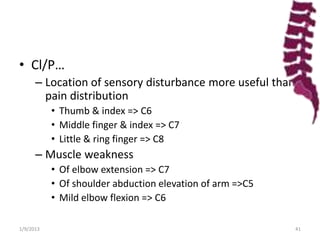
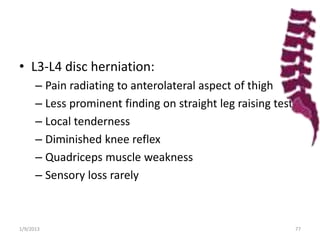
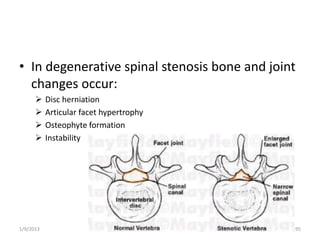
The document outlines degenerative spinal disorders, focusing on cervical and lumbar disc diseases. It details the anatomy, clinical presentations, and various manifestations such as cervical spondylosis, herniation, and spinal stenosis. Management strategies including conservative treatments and surgical interventions like foraminotomy and anterior cervical discectomy are also discussed.