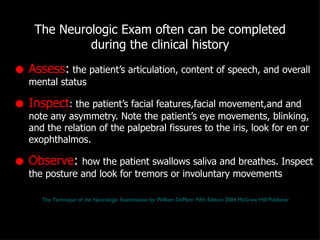
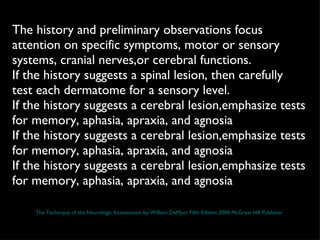
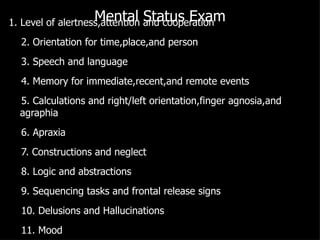
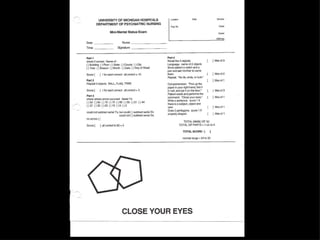
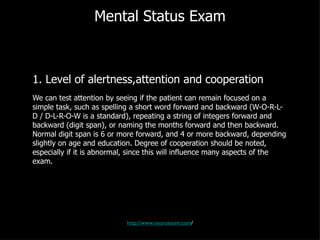
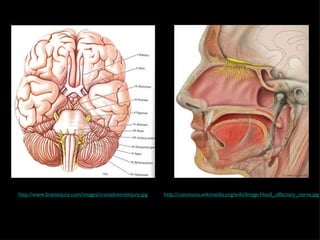
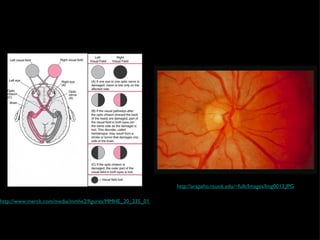
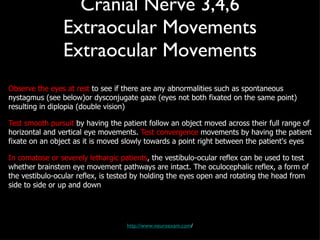
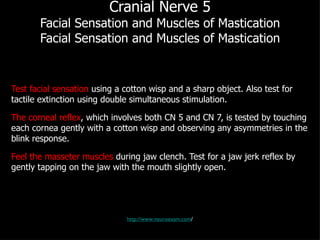
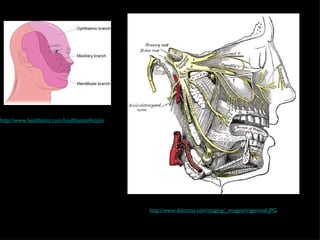
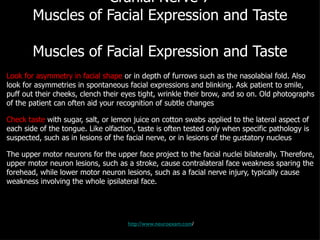
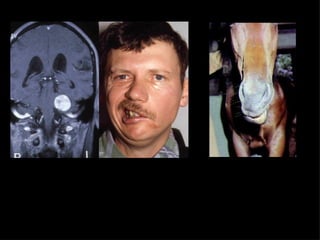
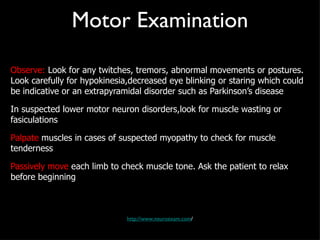
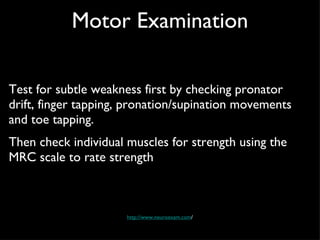
The document provides guidance on performing a neurologic examination, beginning with the mental status exam and covering tests of the cranial nerves and other neurologic functions. It emphasizes that the history guides the focused examination and different pathologies require evaluating specific symptoms, motor or sensory systems. Tests are described to assess functions like orientation, memory, speech, eye movements, facial sensation and expression, hearing, and balance. References to additional resources on neurologic examination techniques are also provided.