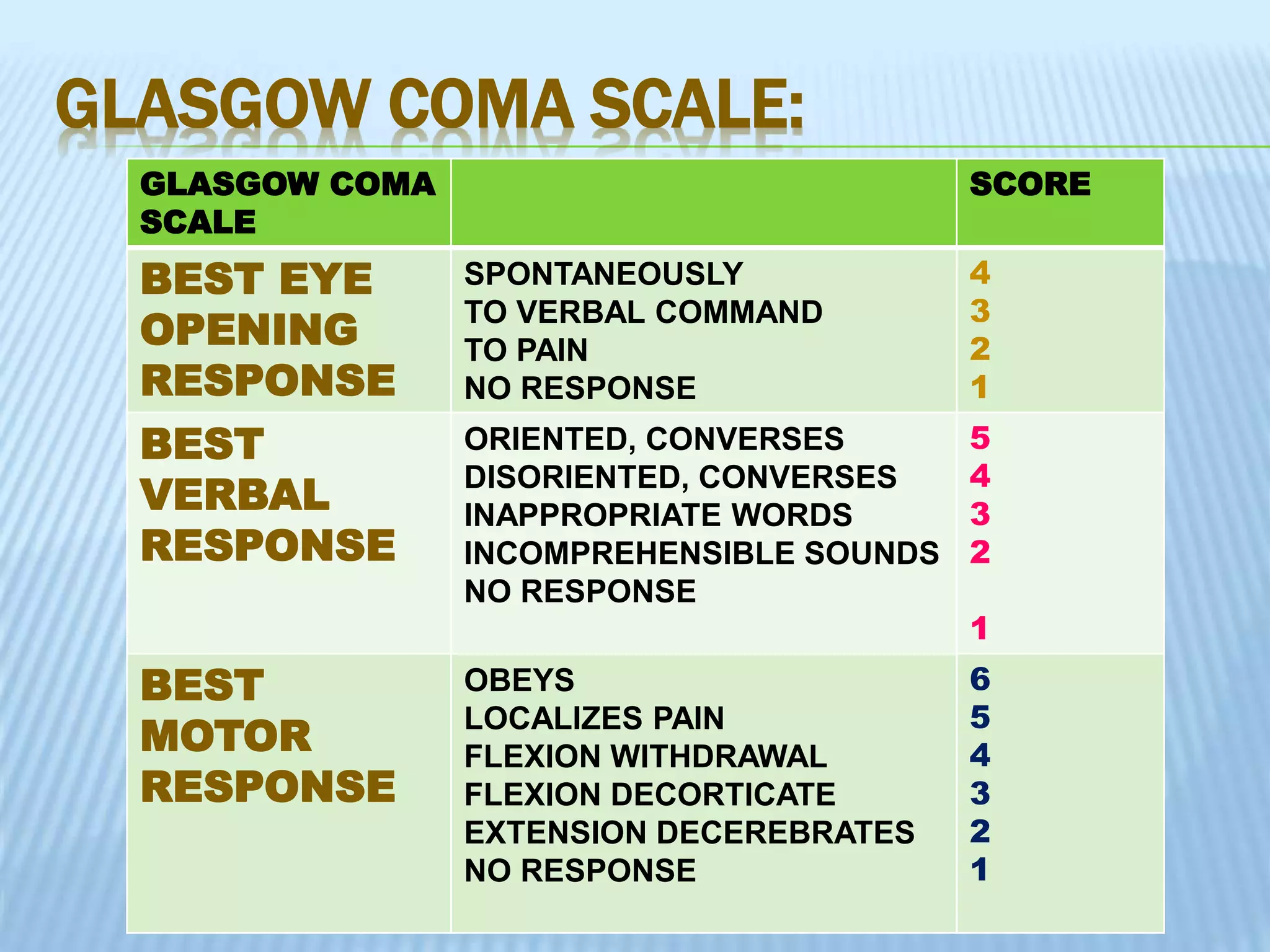
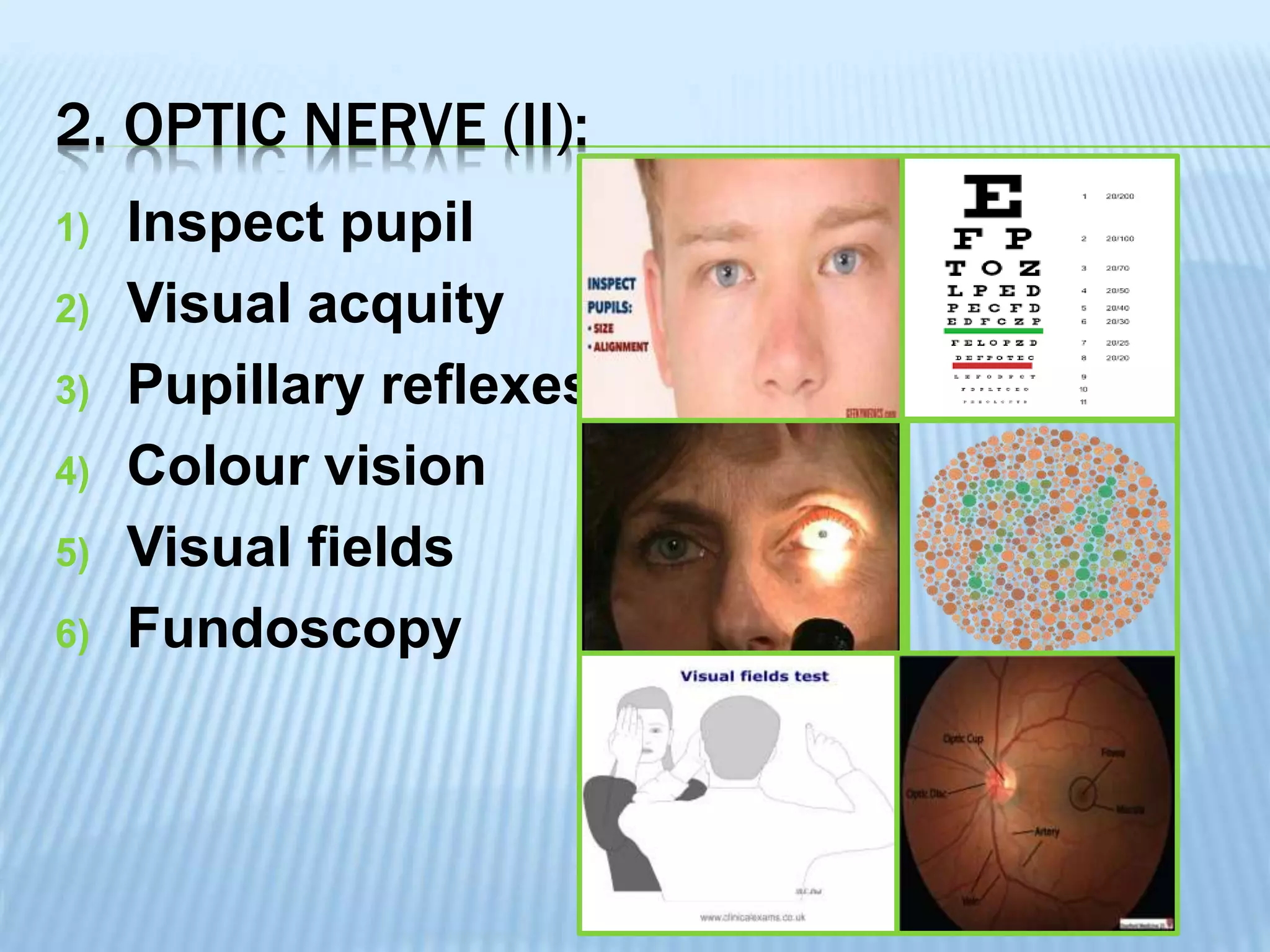
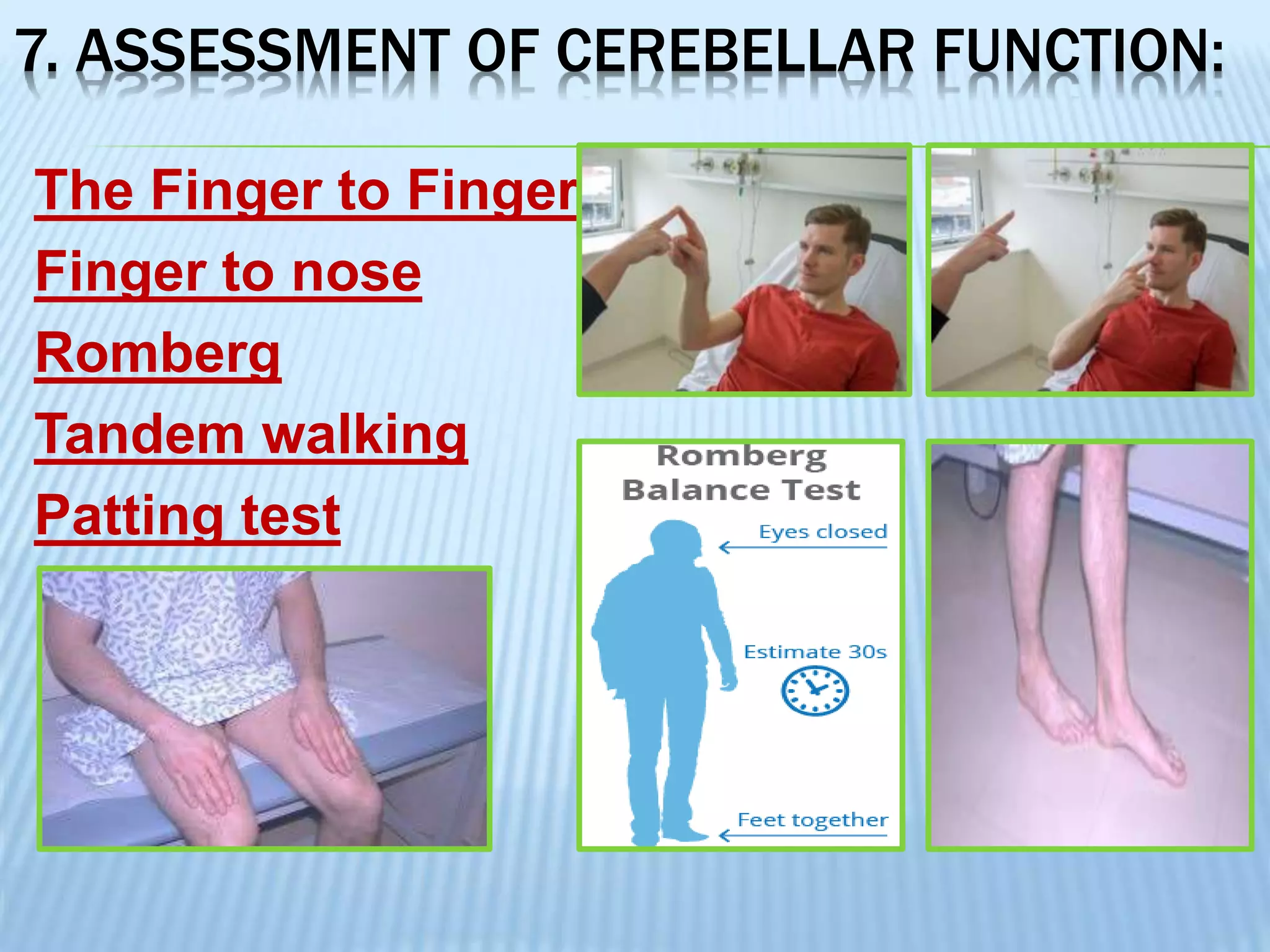
The document outlines a comprehensive neurological assessment process, detailing the components of a neurological examination and the necessary equipment. It provides information on evaluating patient history, consciousness levels, mental status, and cranial nerve functions, along with various tests for motor and sensory functions. The document serves as a guide for identifying neurological issues and is relevant for patients with conditions such as meningitis, head injuries, and coma.