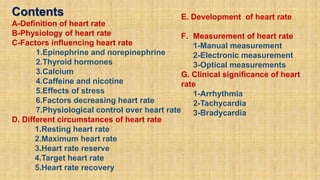
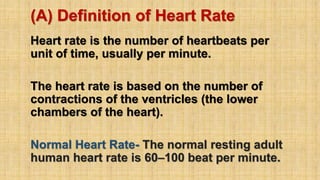
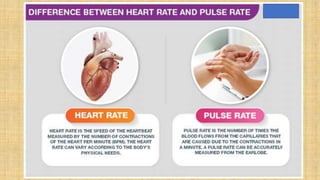
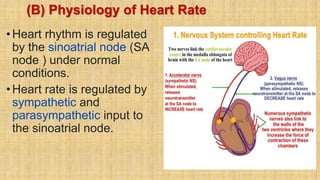
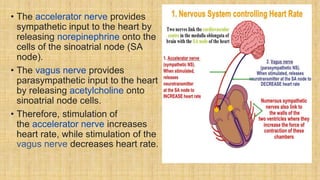
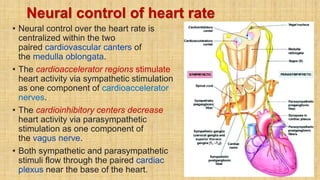
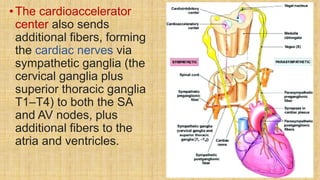
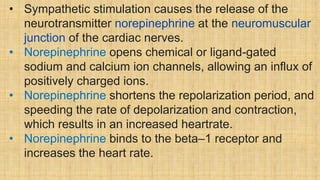
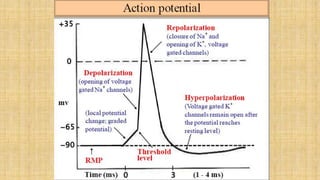
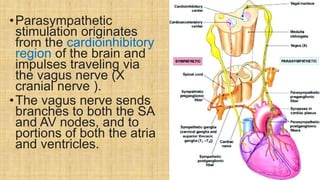
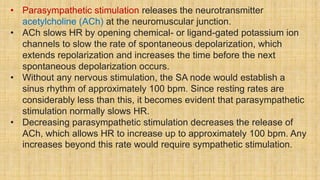
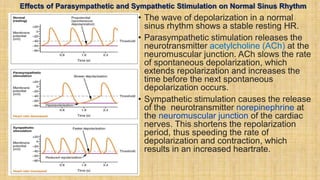
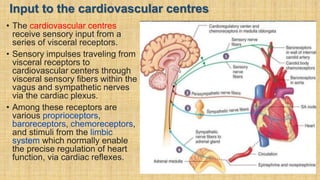
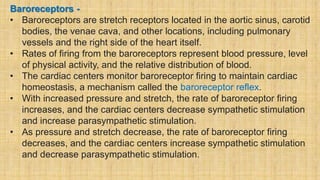
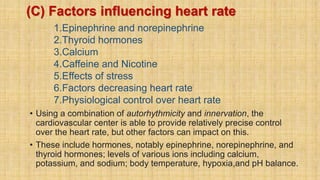
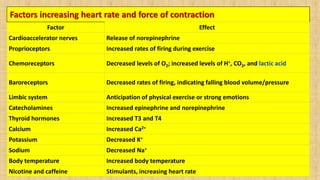
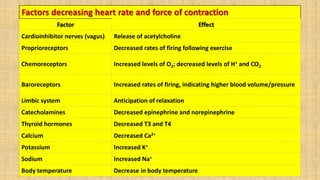
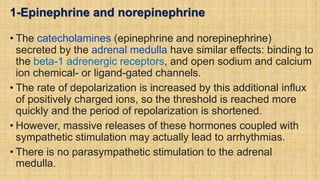
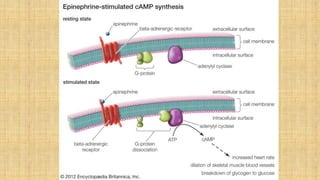
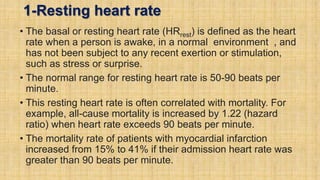
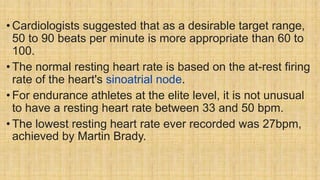
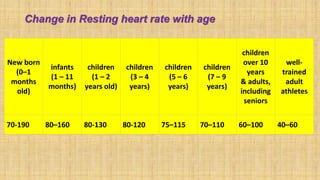
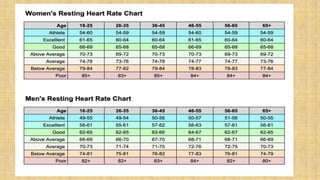
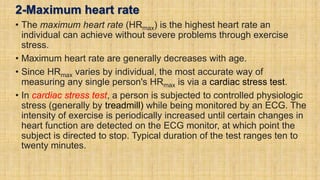
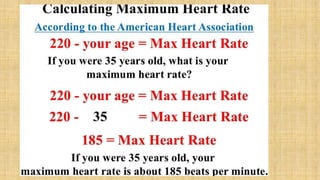
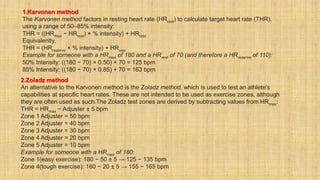
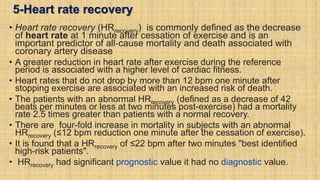
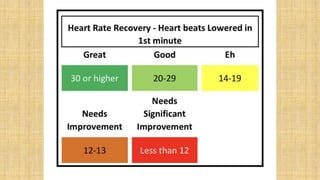
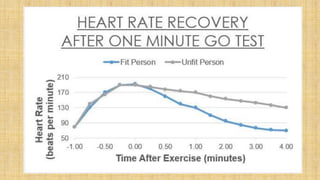
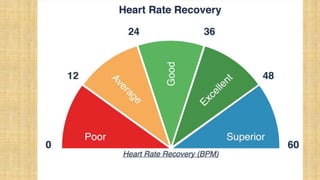
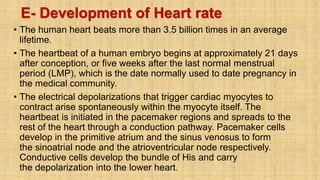
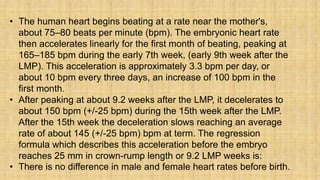
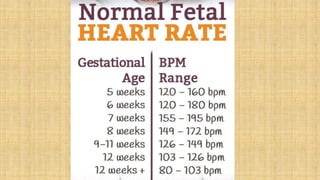
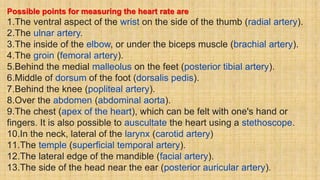
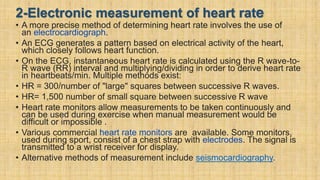
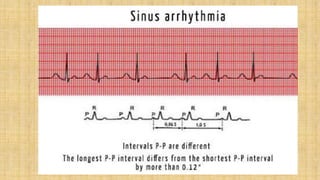
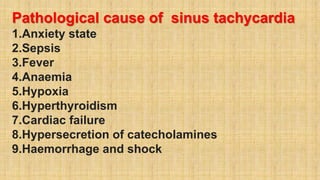
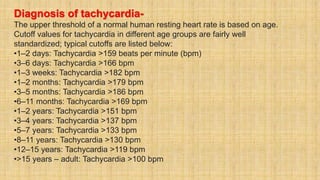
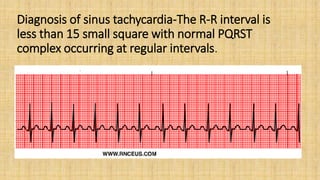
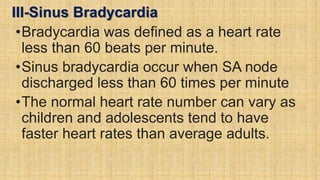
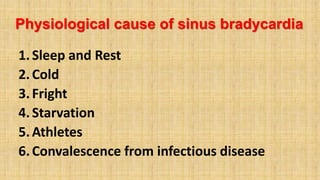
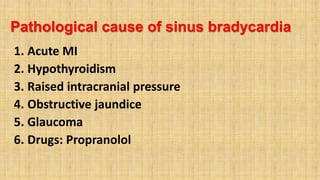
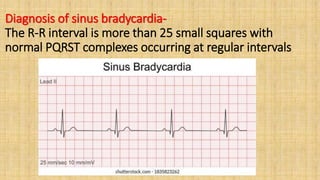
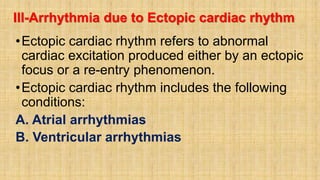
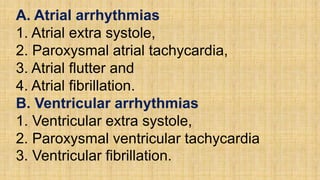
The document provides a comprehensive overview of heart rate, including its definition, physiology, and factors influencing it such as hormones, stress, and age. It discusses different circumstances of heart rate such as resting, maximum, and recovery rates, along with methods for measurement and clinical significance like arrhythmia and tachycardia. The document emphasizes the complex regulation of heart rate through neural inputs, hormonal actions, and physiological responses to various stimuli.