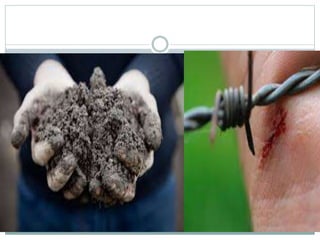
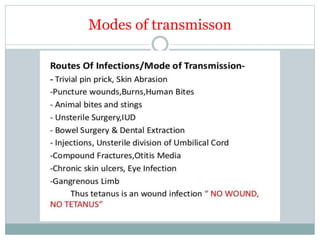
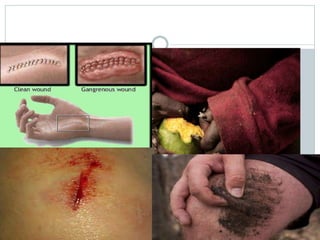
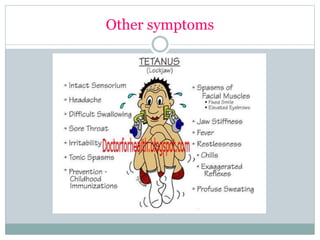
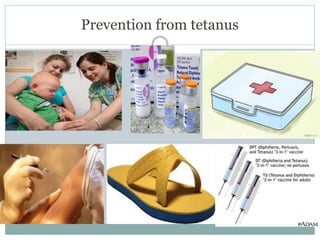
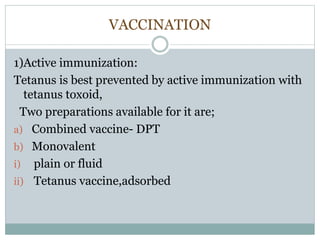
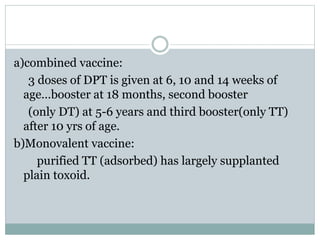
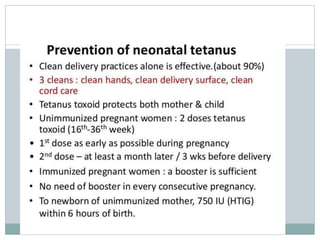
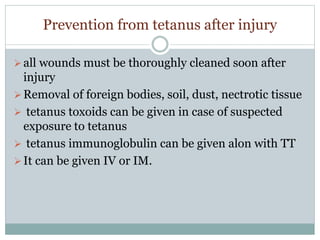
Tetanus is caused by the bacterium Clostridium tetani which produces a toxin that affects the nervous system. The spores can be found in soil and dust and enter the body through wounds. The toxin causes painful muscle spasms starting with the jaw and potentially affecting breathing. Tetanus is prevented through active immunization with tetanus toxoid vaccines as part of routine childhood immunization schedules with boosters recommended every 10 years. For wound management, thorough cleaning and antibiotics may be given along with a tetanus toxoid booster or immunoglobulin for non-immunized individuals.