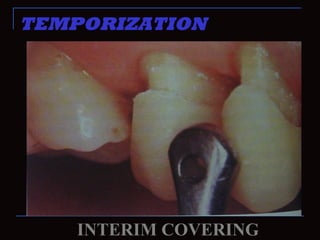
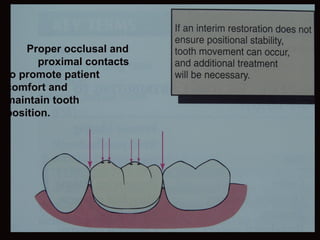
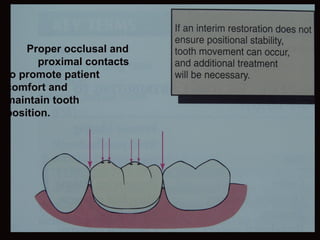
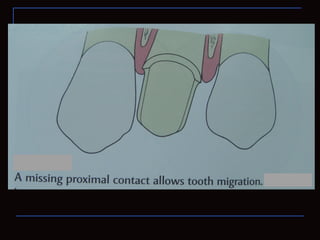
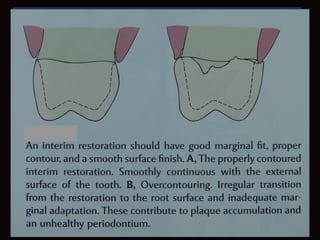
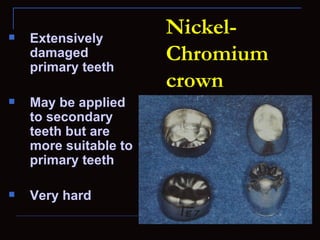
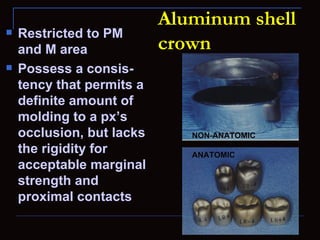
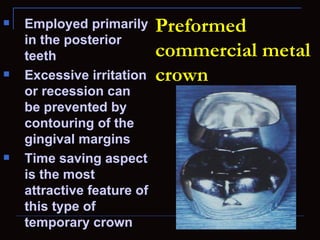
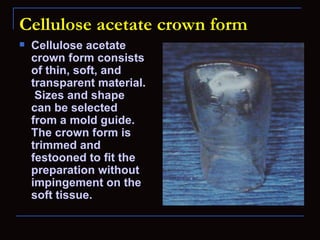
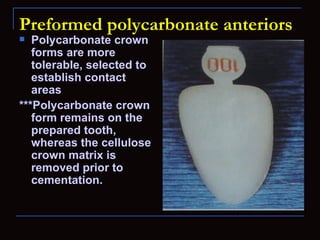
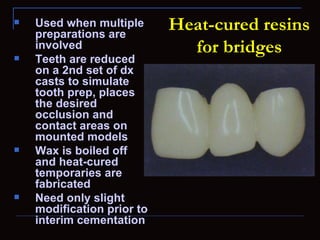
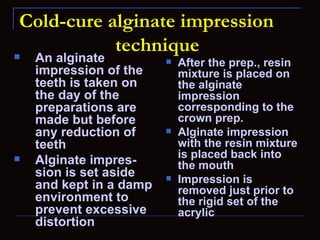
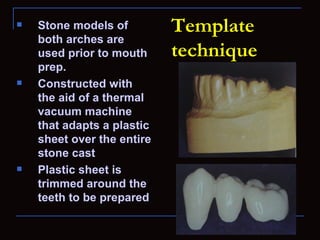
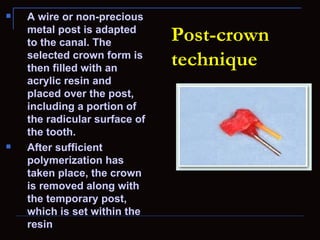
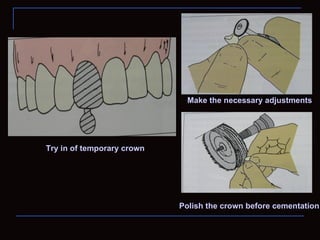
This document discusses temporization, or the placement of interim restorations. It describes the importance of temporization for maintaining tooth vitality and position. Common problems with temporization include underestimating fabrication time and delays replacing temporaries with permanent restorations. The document outlines several techniques for fabricating temporary crowns from various materials to address these issues, including metal, acrylic, and polycarbonate crowns. It also lists cardinal requirements and limitations of temporary crowns.