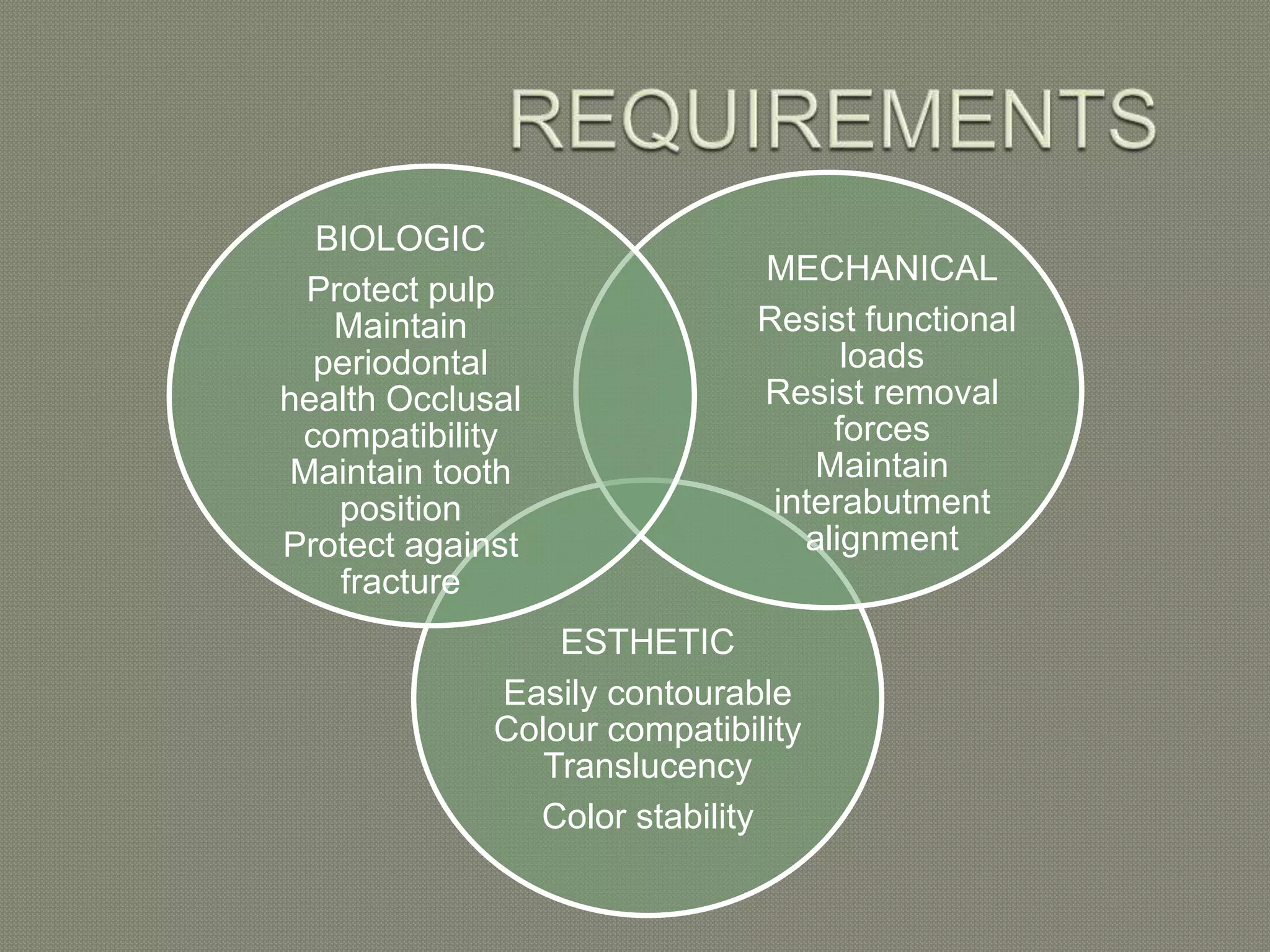
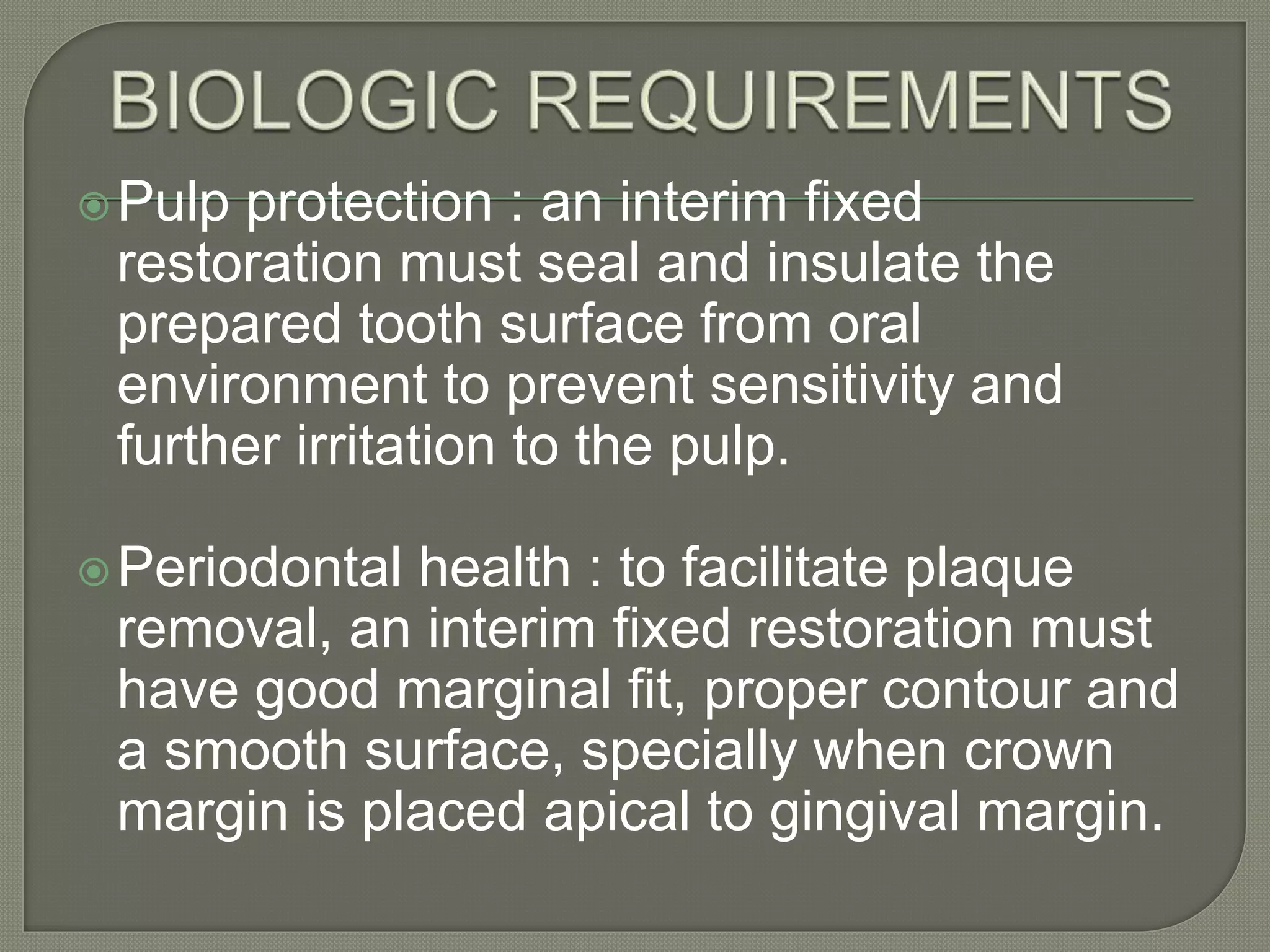
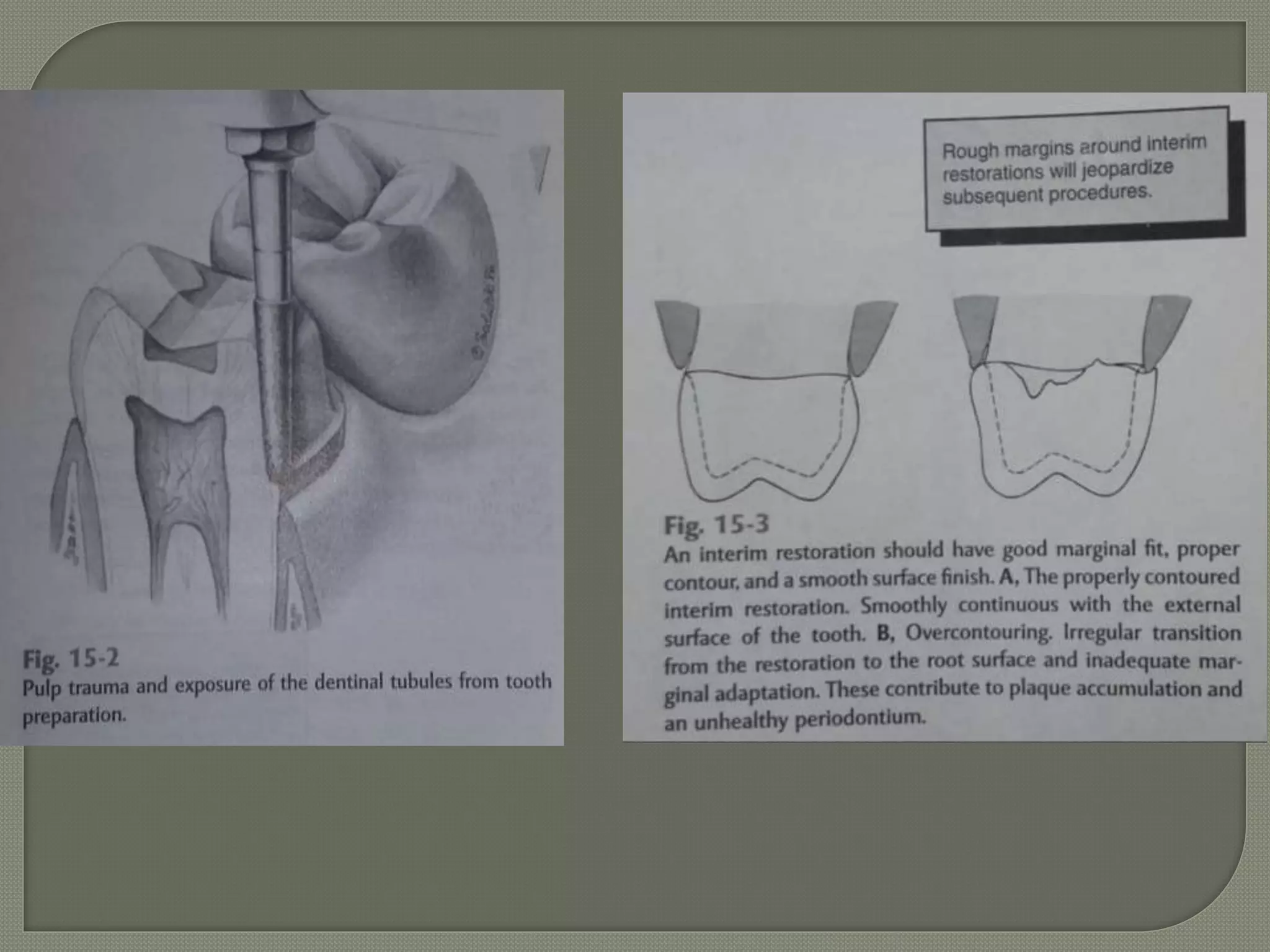
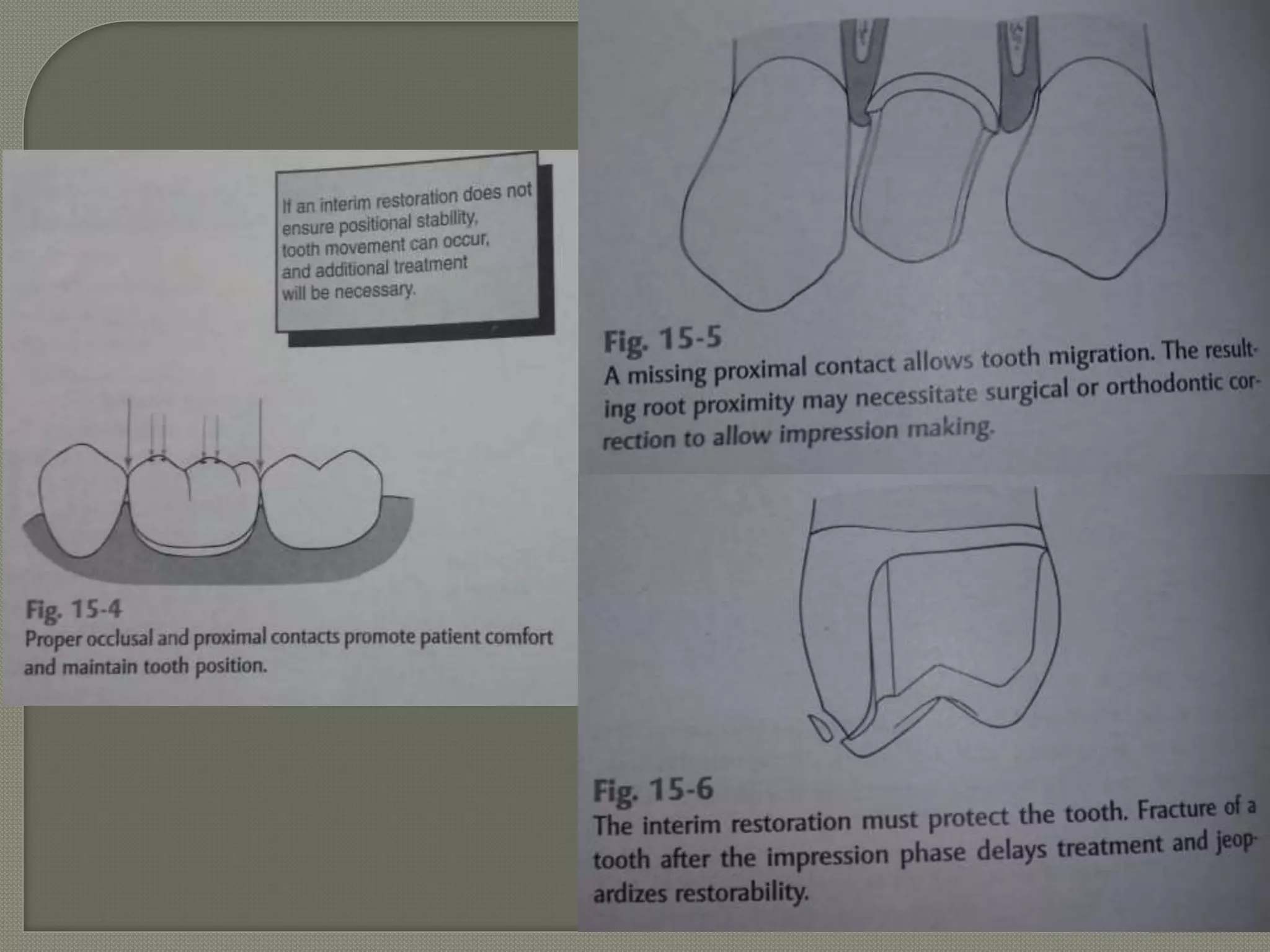
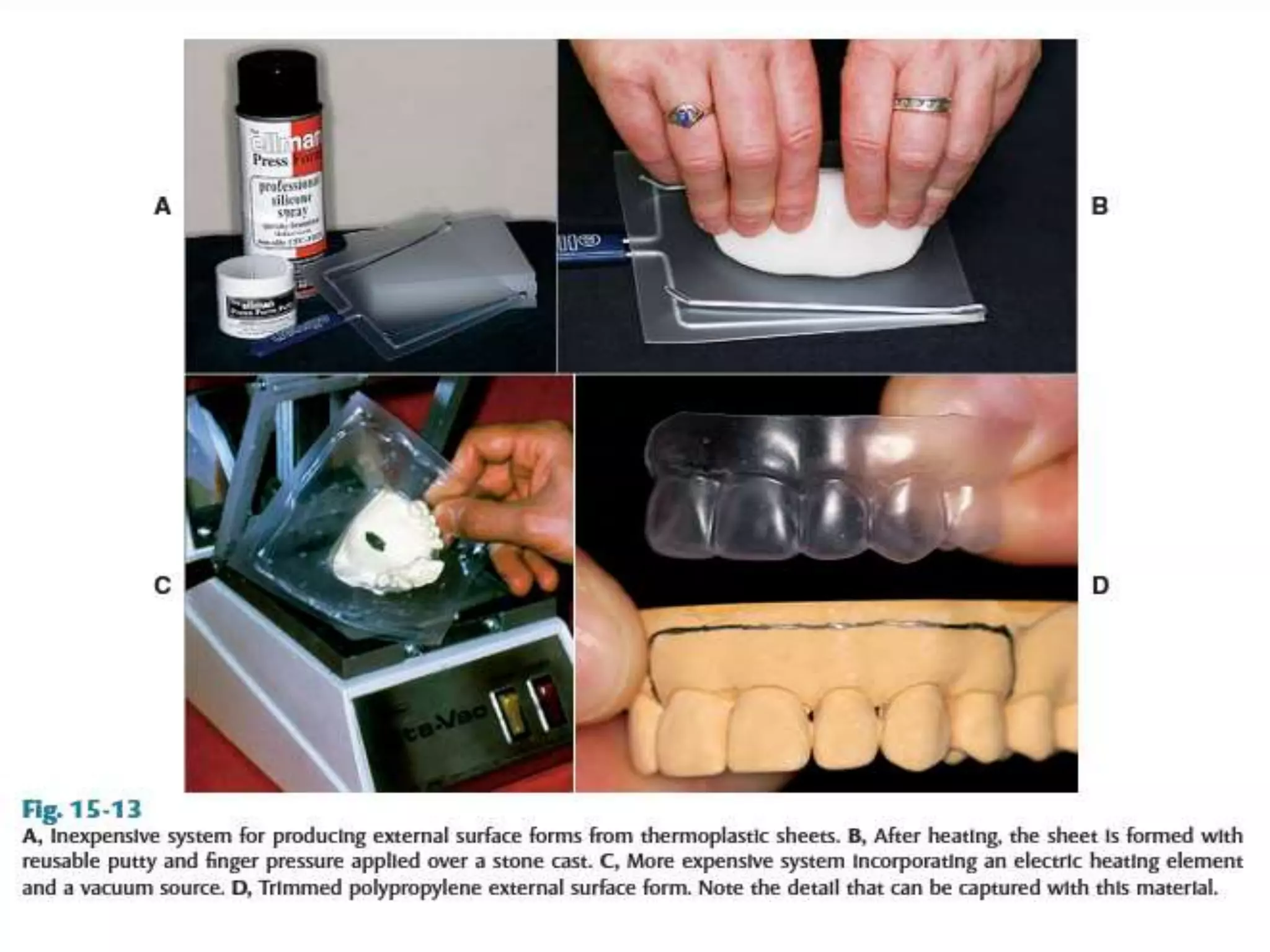
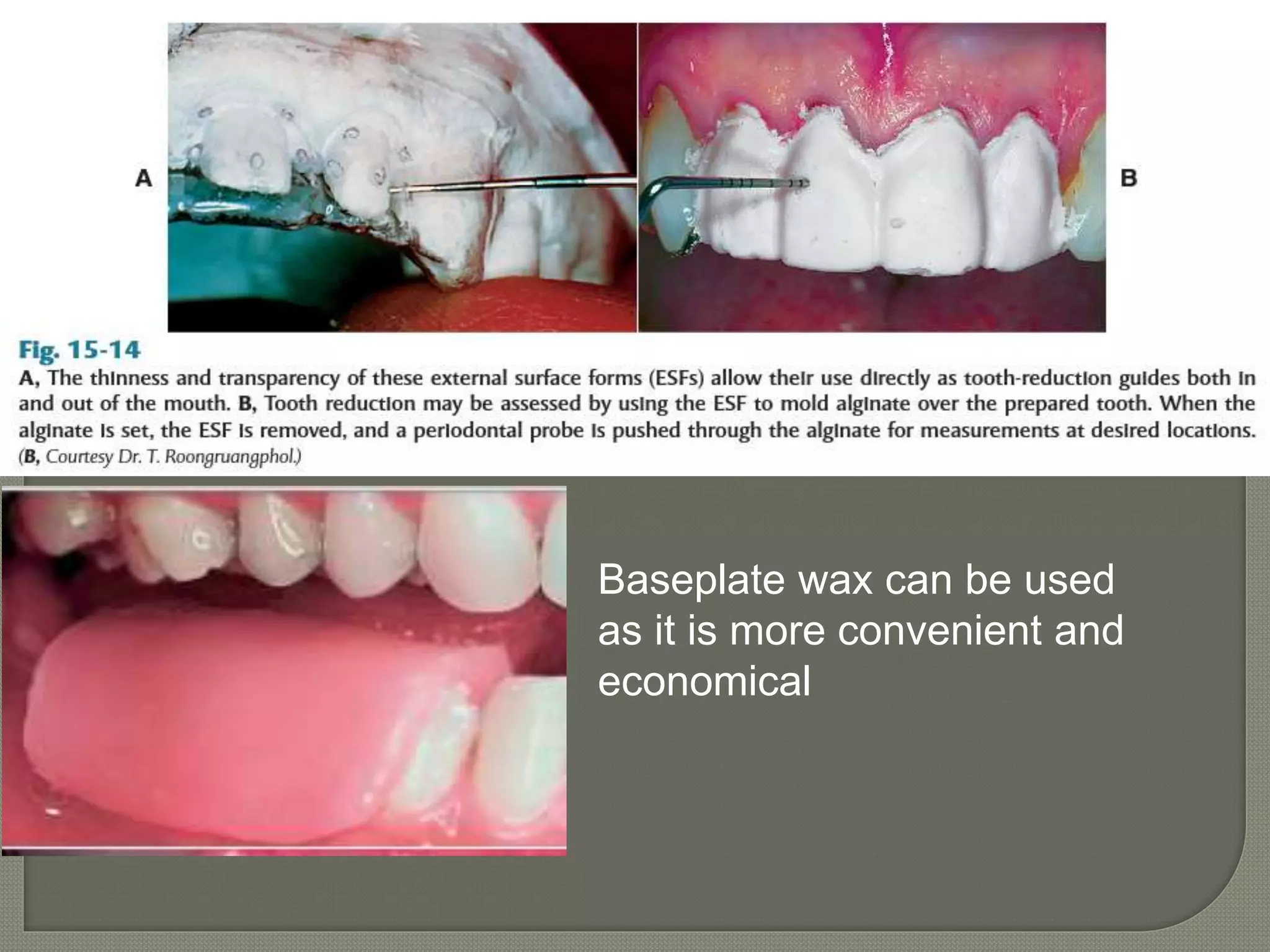
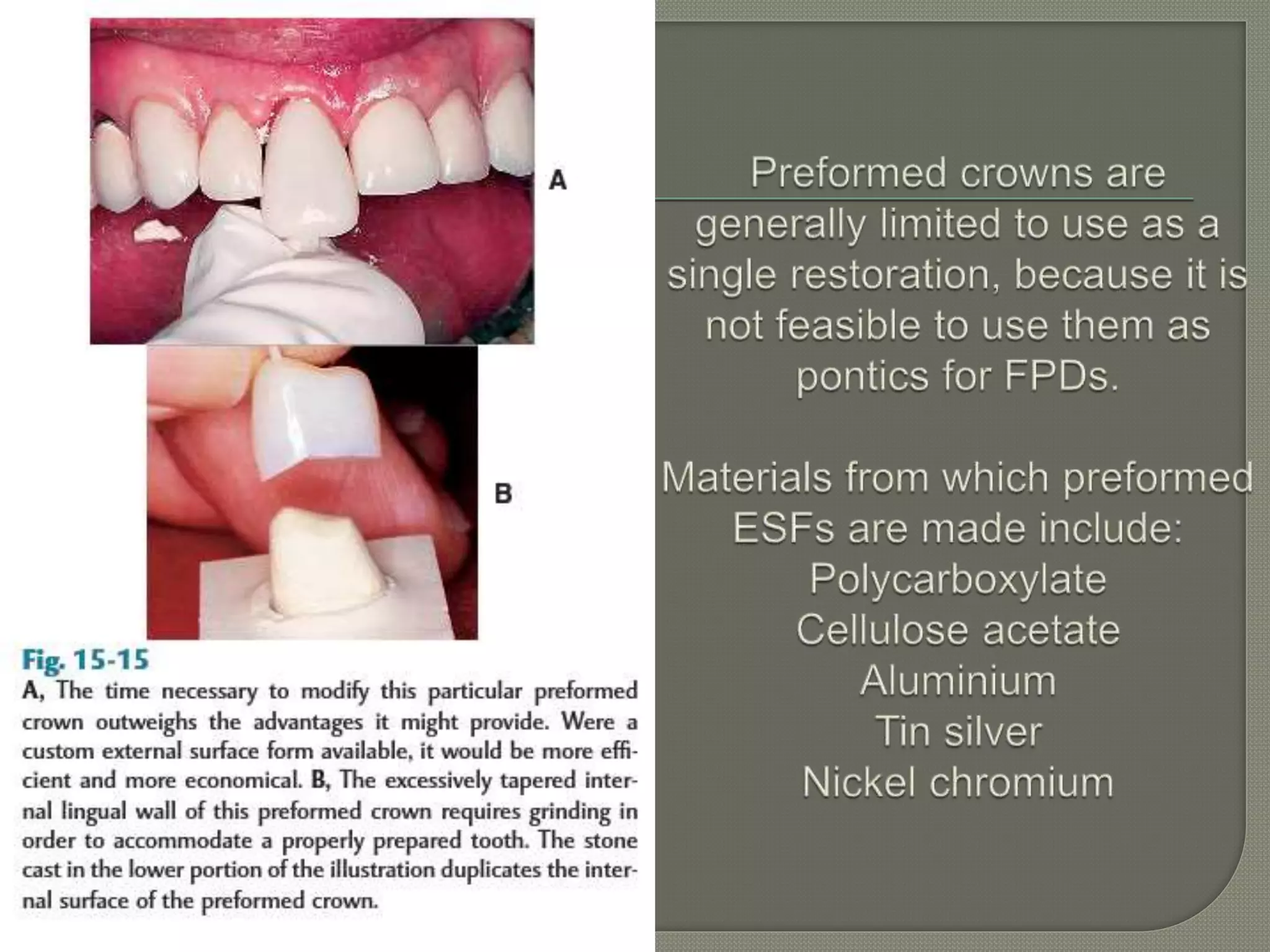
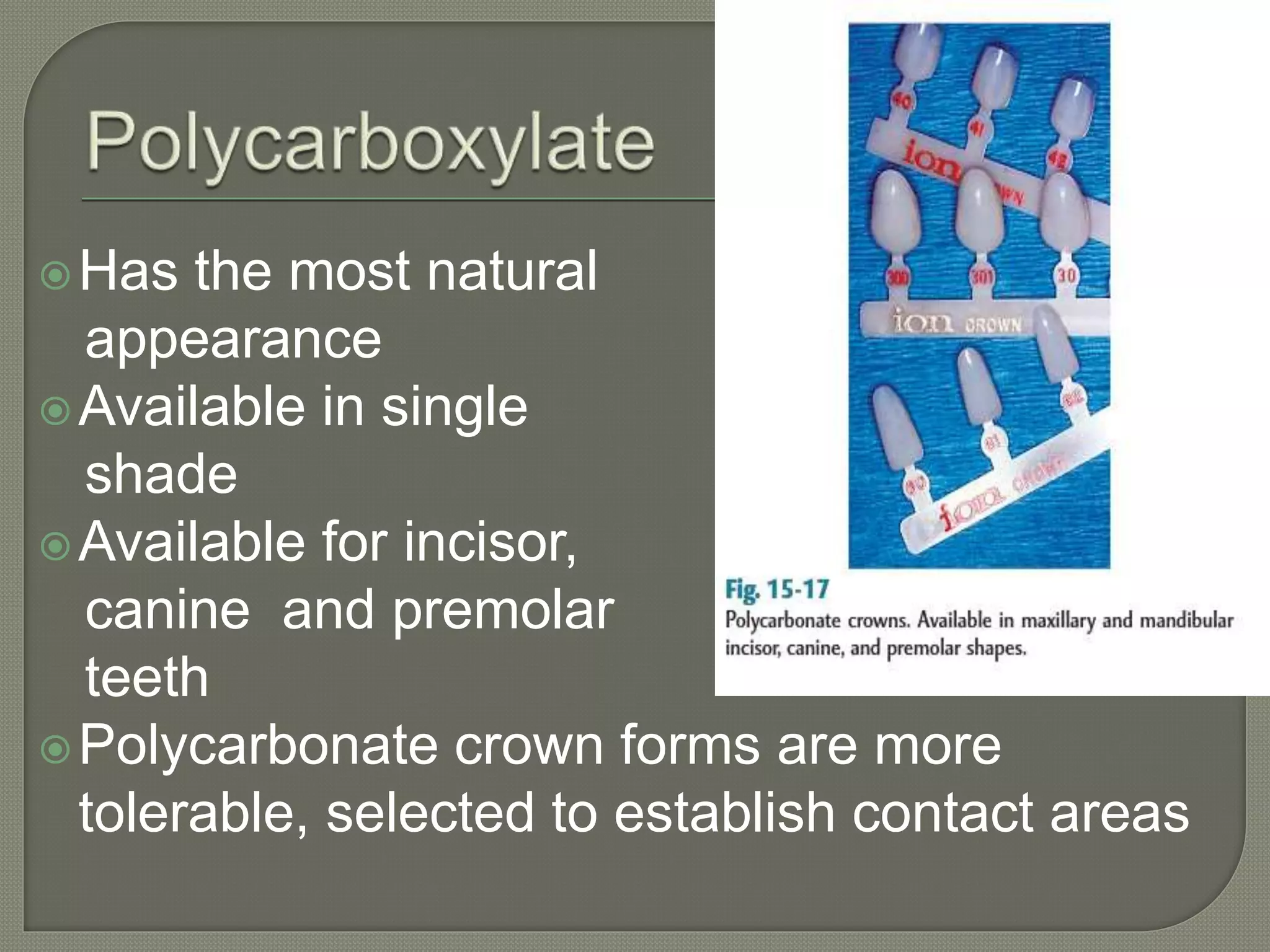
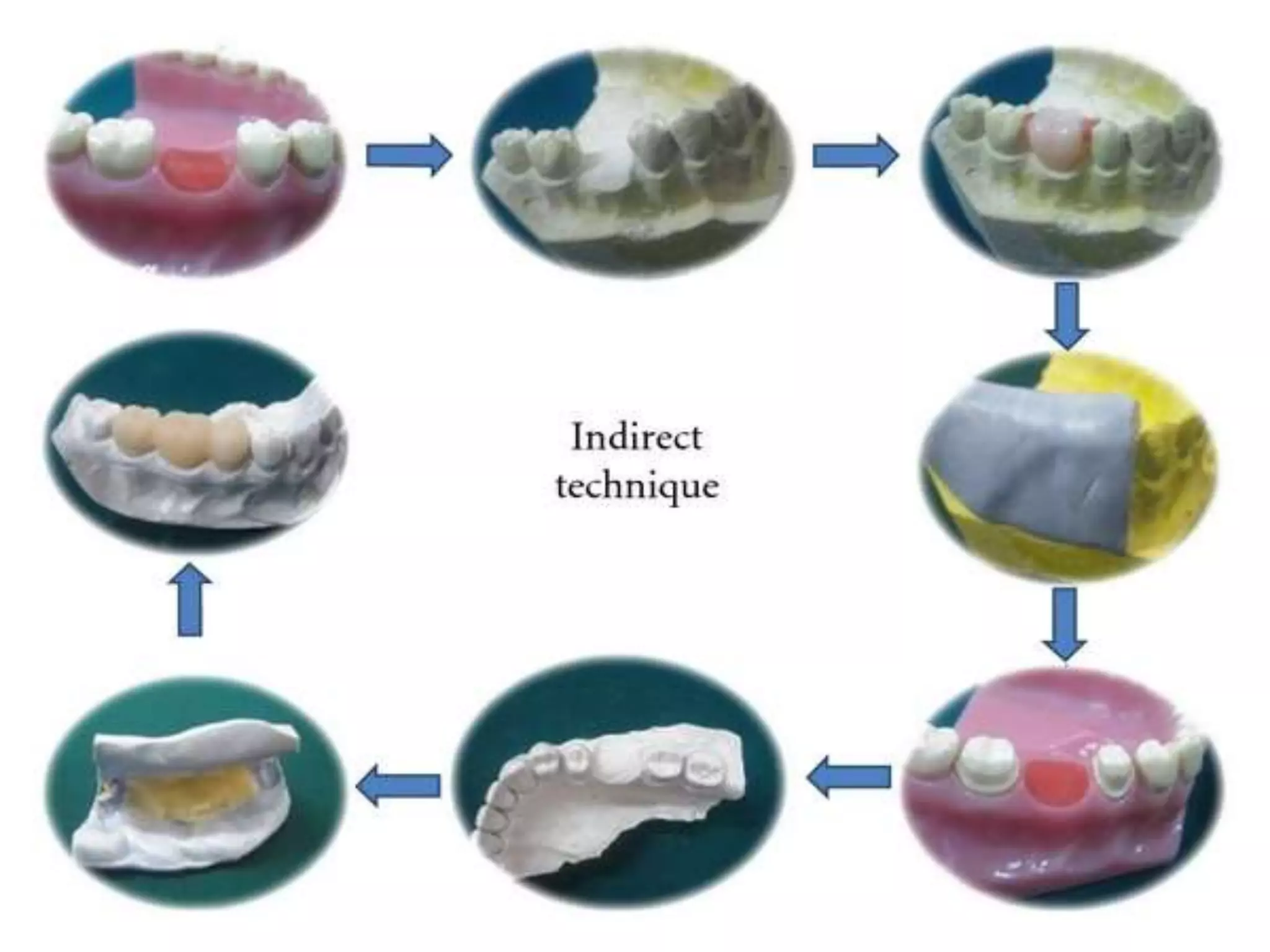
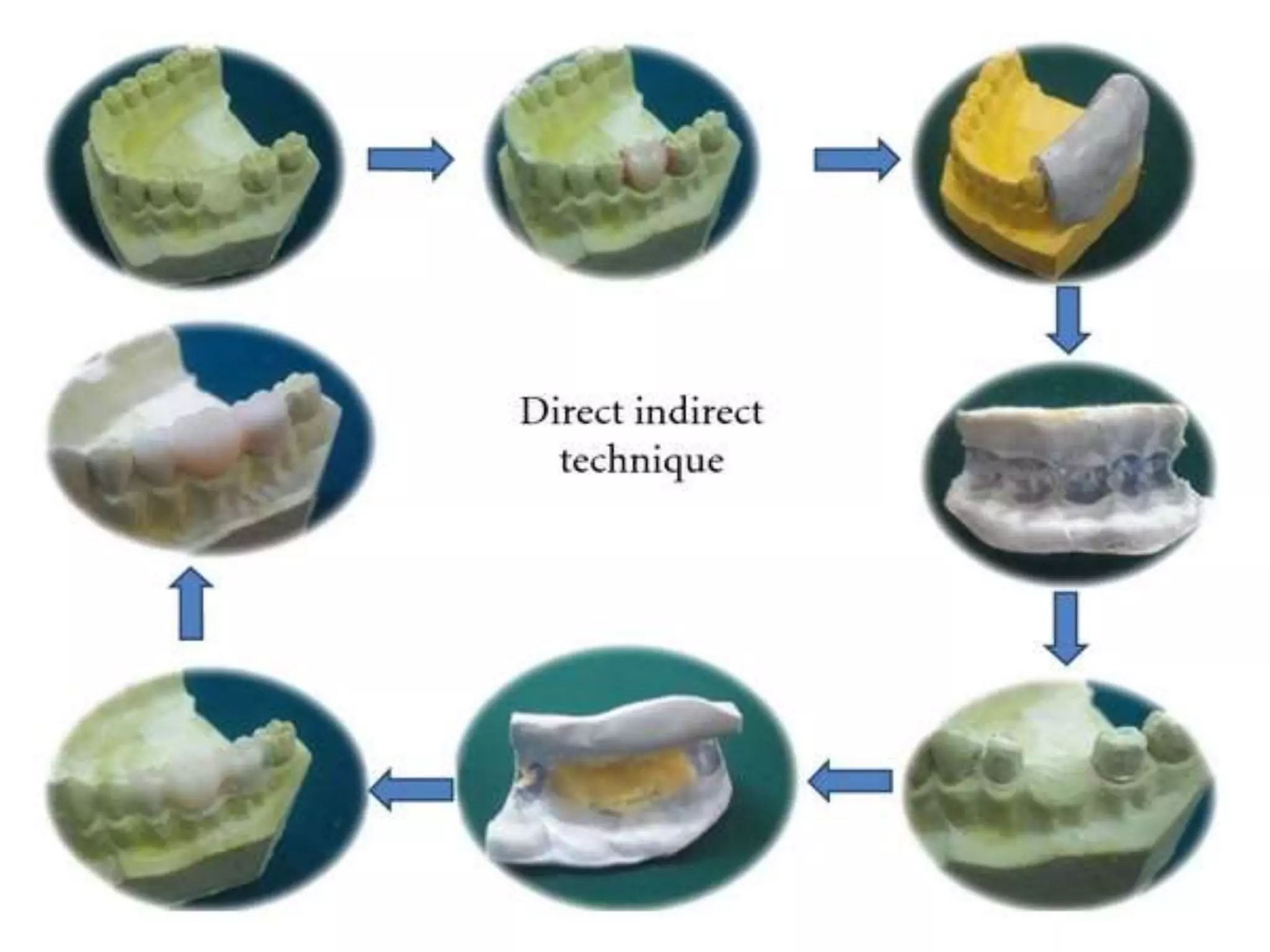
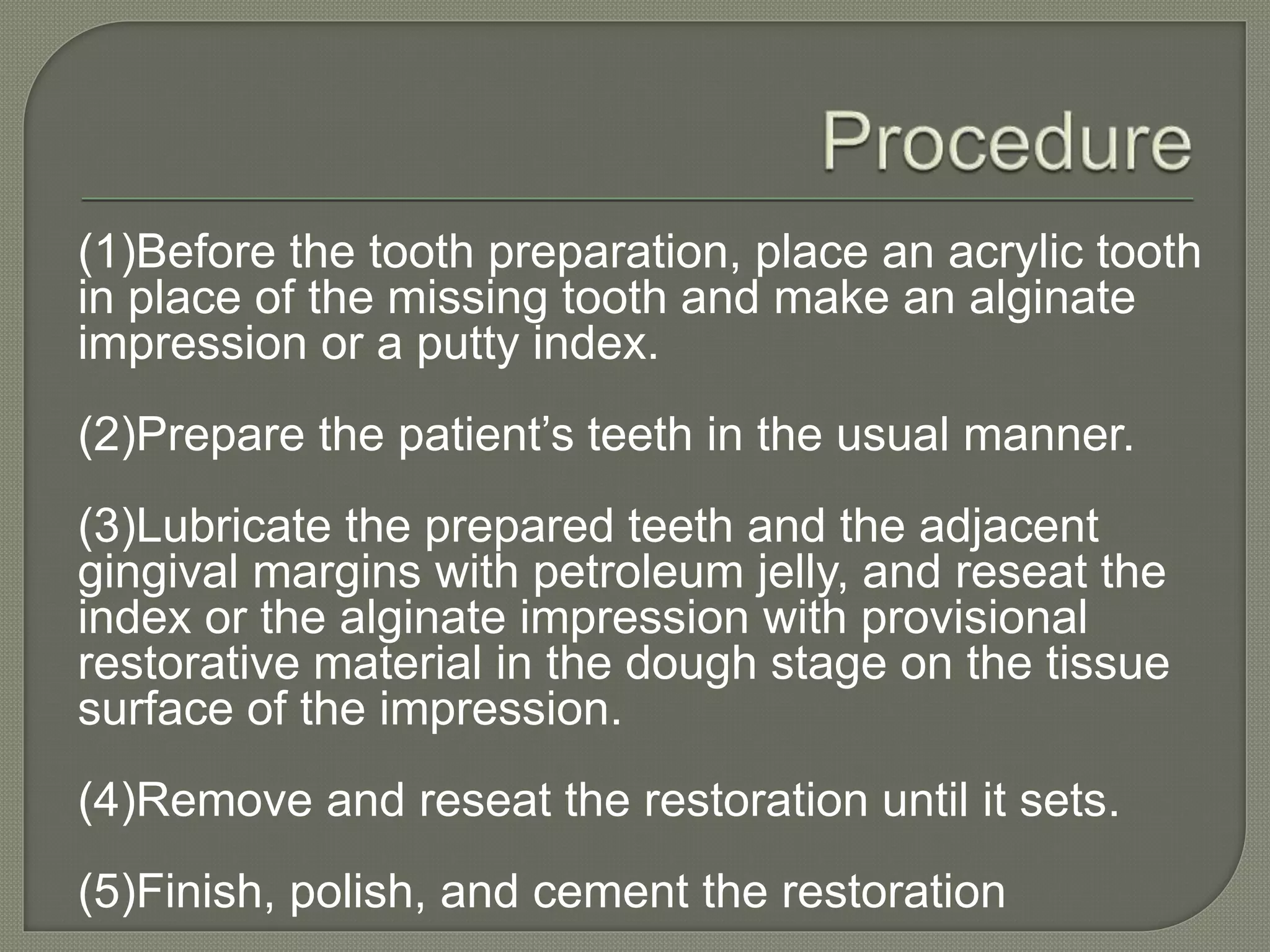
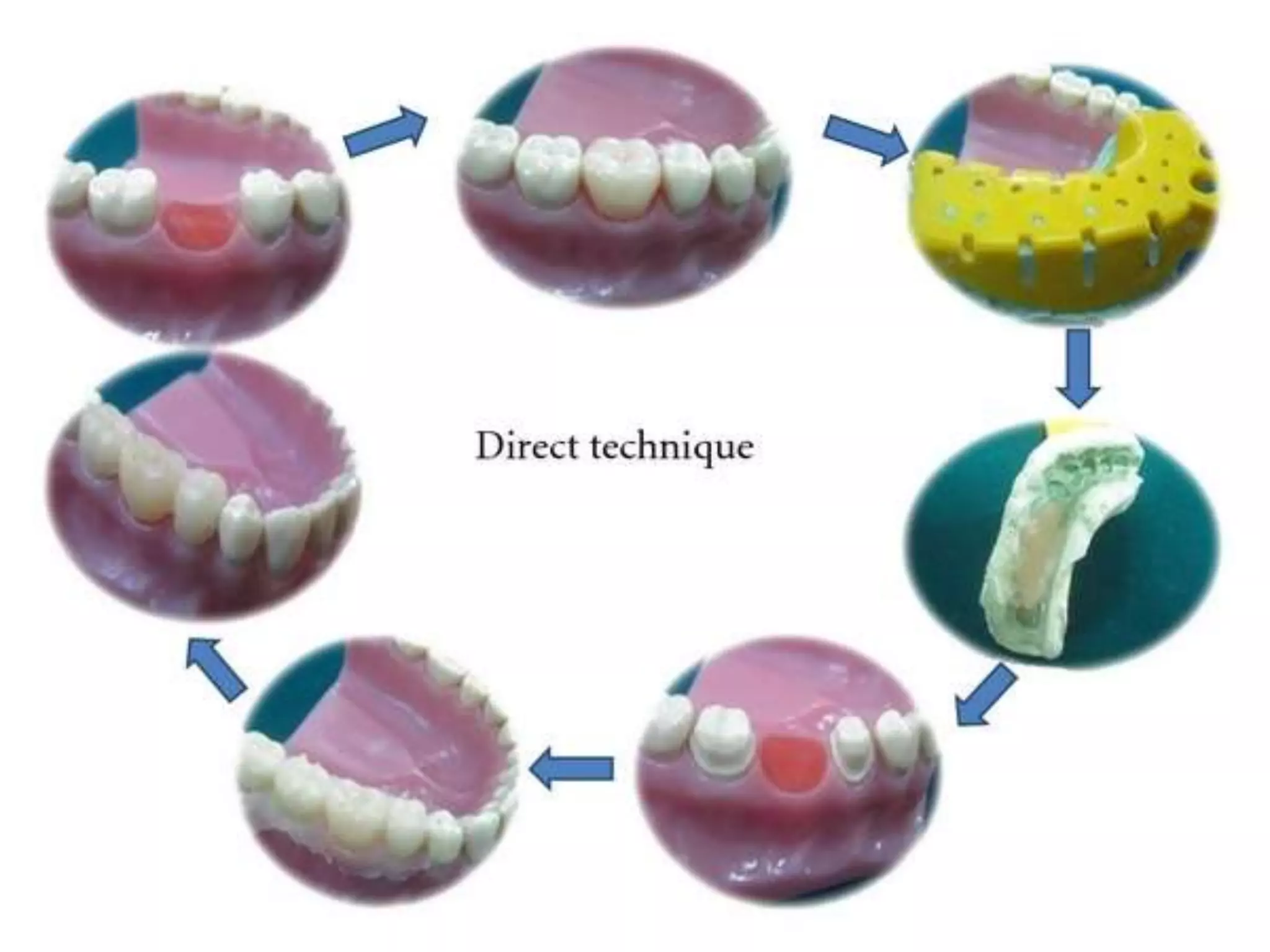
An interim prosthesis is a temporary dental restoration used while determining the effectiveness of a treatment plan or design of a definitive prosthesis. It must satisfy patient and dentist needs by protecting pulp, maintaining oral health, and establishing proper occlusion. Interim restorations can be custom made using impressions or prefabricated shells that are later adjusted. The direct technique forms the restoration directly in the mouth while indirect techniques use models to improve fit and reduce risks.