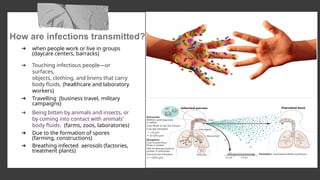
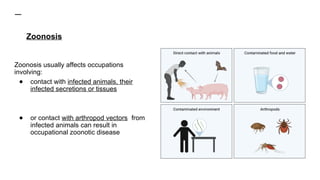
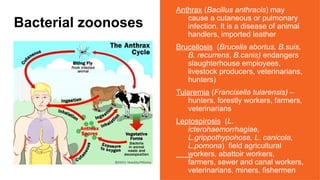
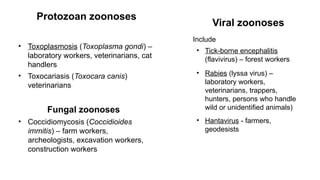
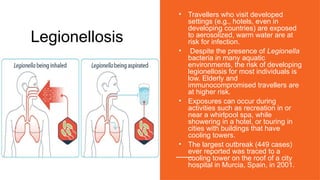
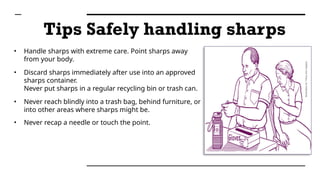
The document provides a comprehensive overview of occupational infections, defined as diseases resulting from work-related exposure to microbial agents, categorized into anthroponosis and zoonoses. It outlines transmission methods, common infectious diseases related to different occupations, and emphasizes preventive measures like vaccination, hygiene, and proper handling of sharps. Case studies illustrate real-world scenarios highlighting the risks and necessary precautions for healthcare workers to mitigate infection risks.