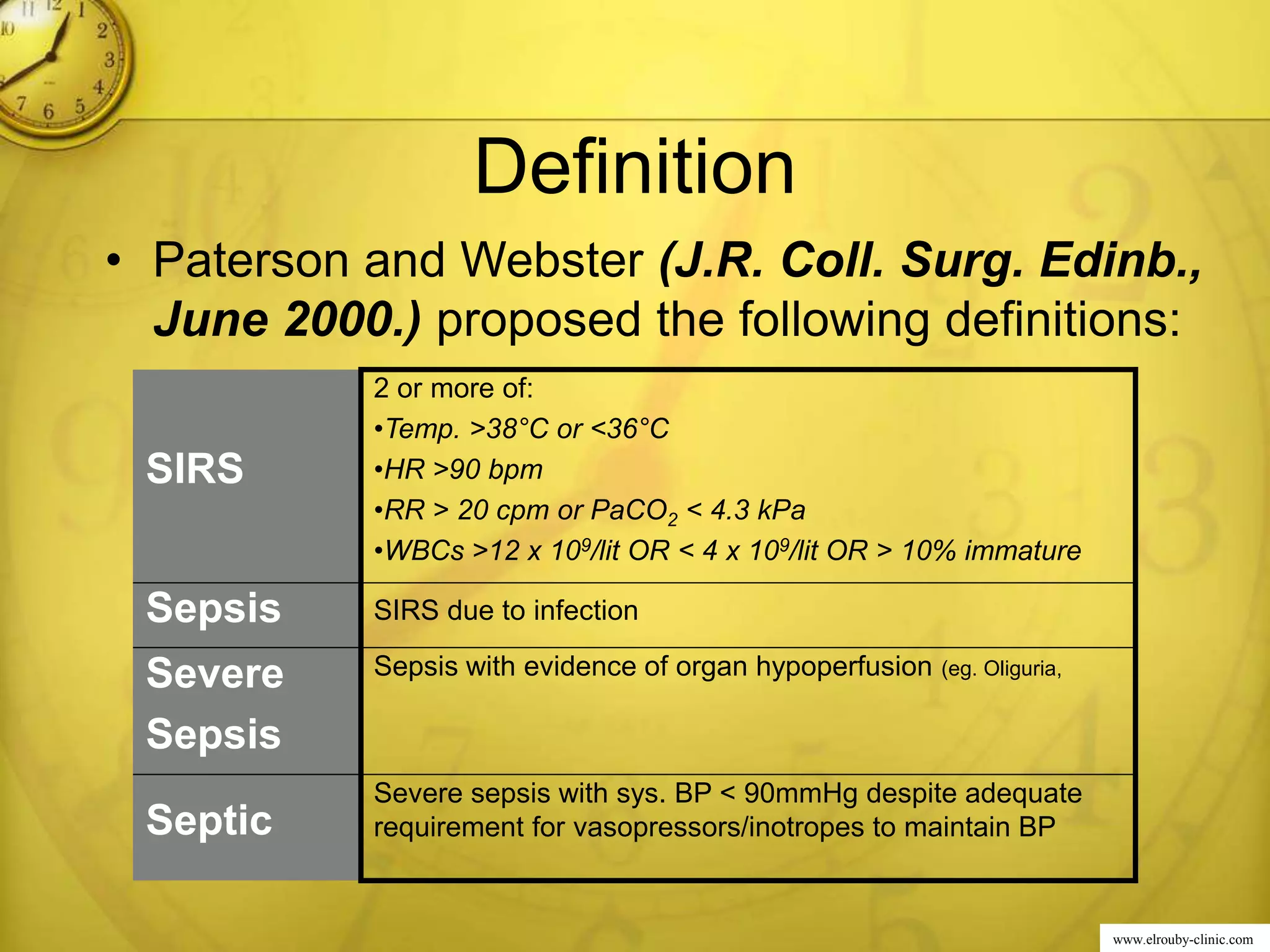
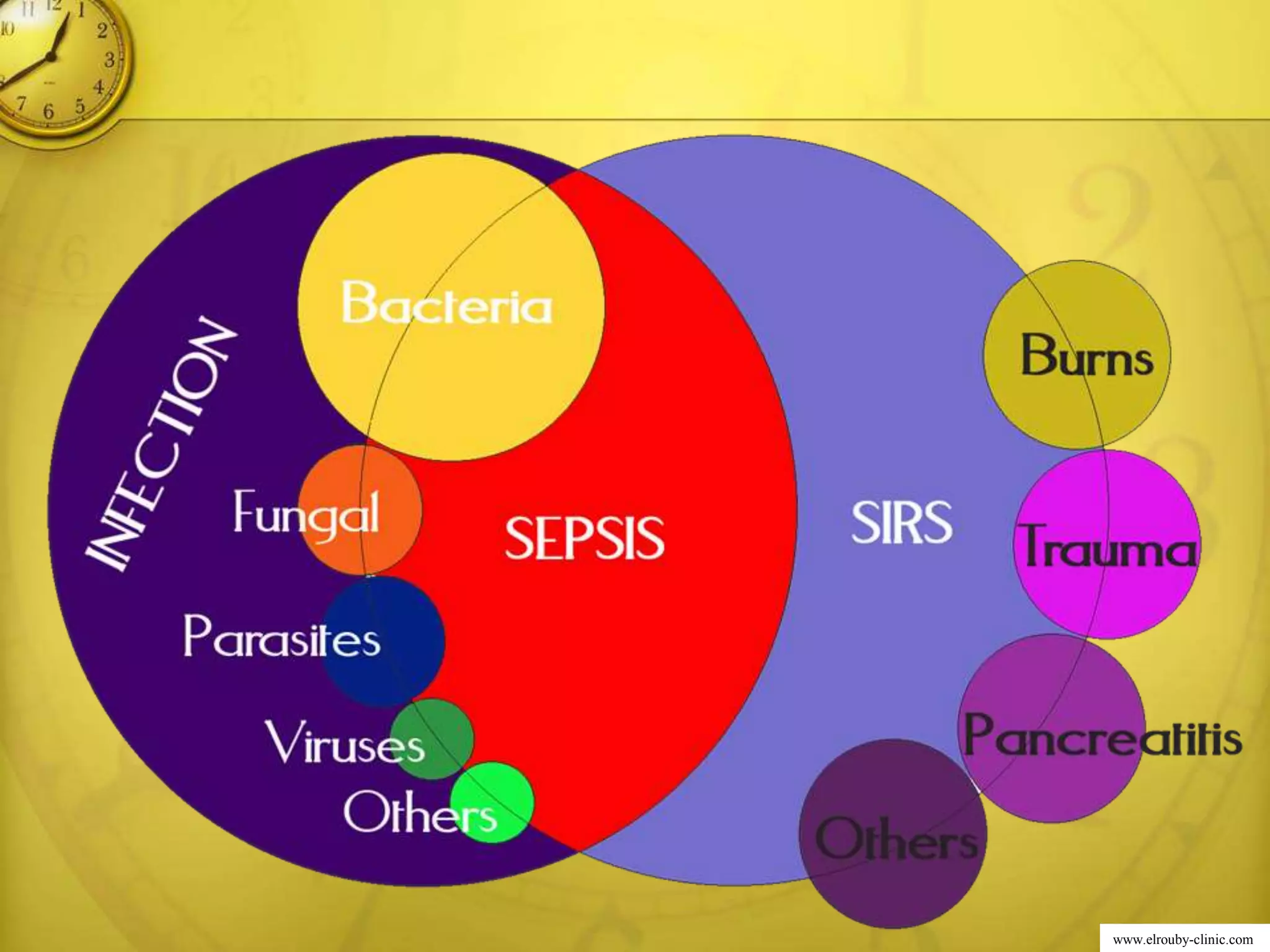
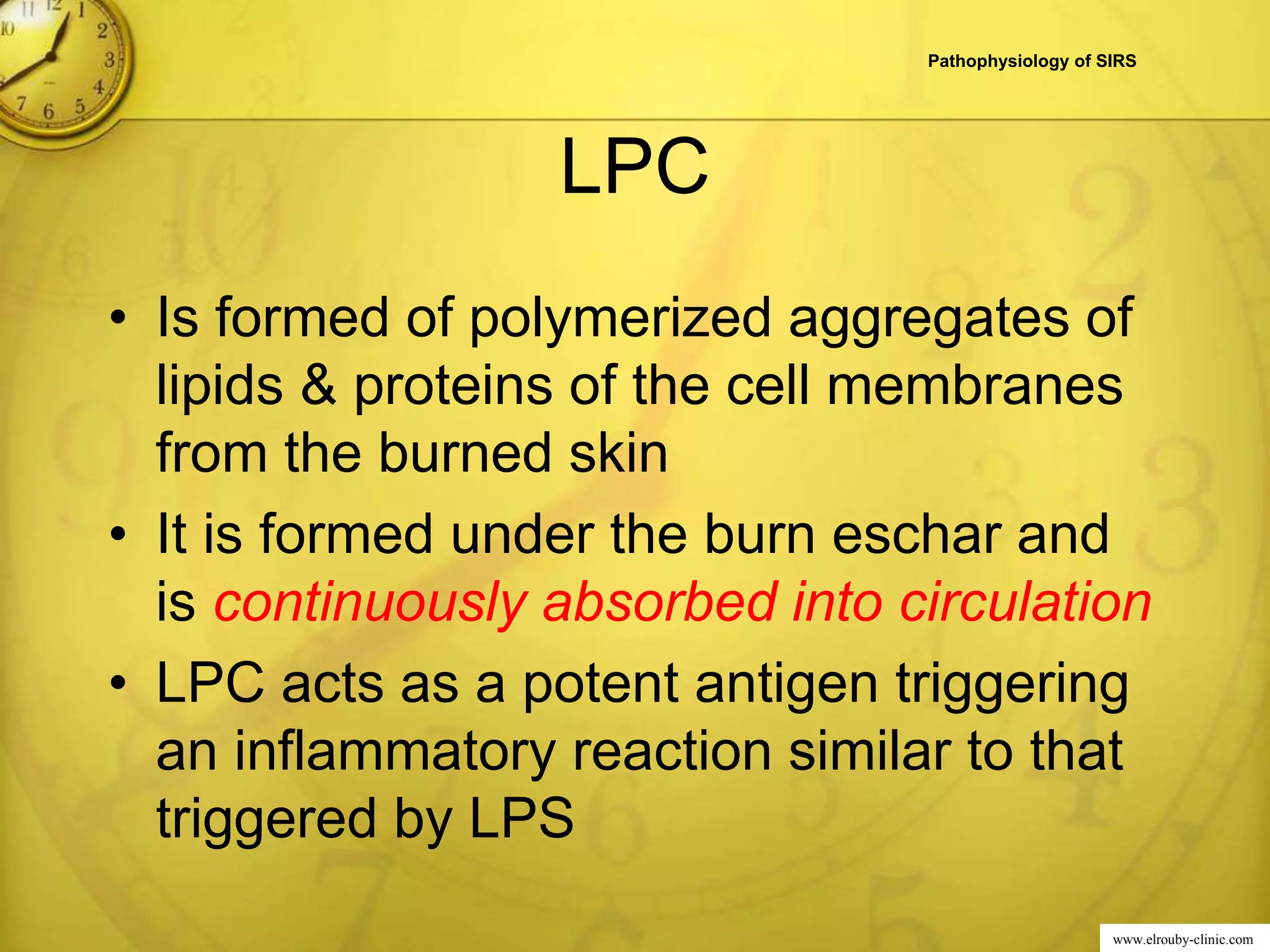
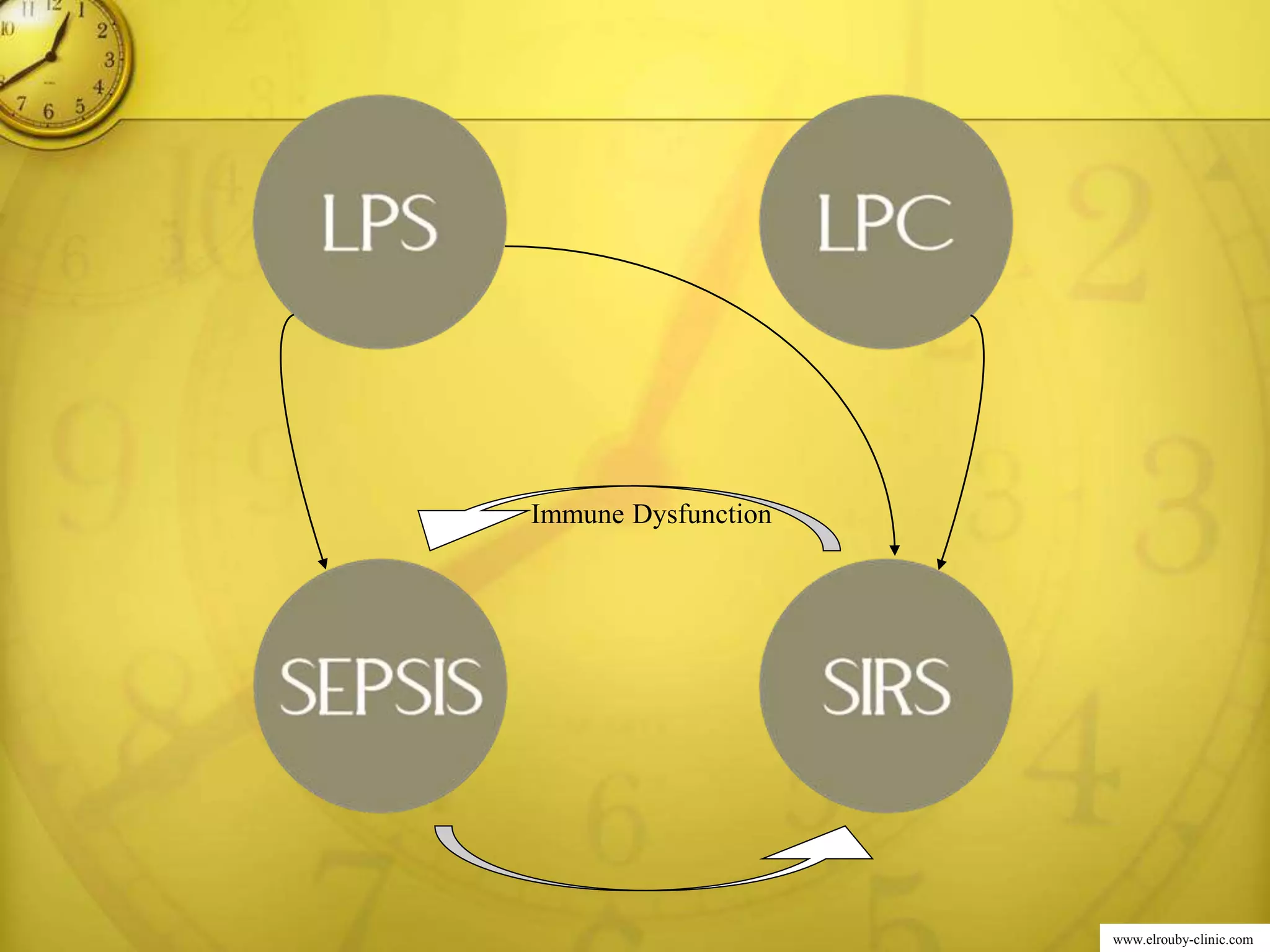
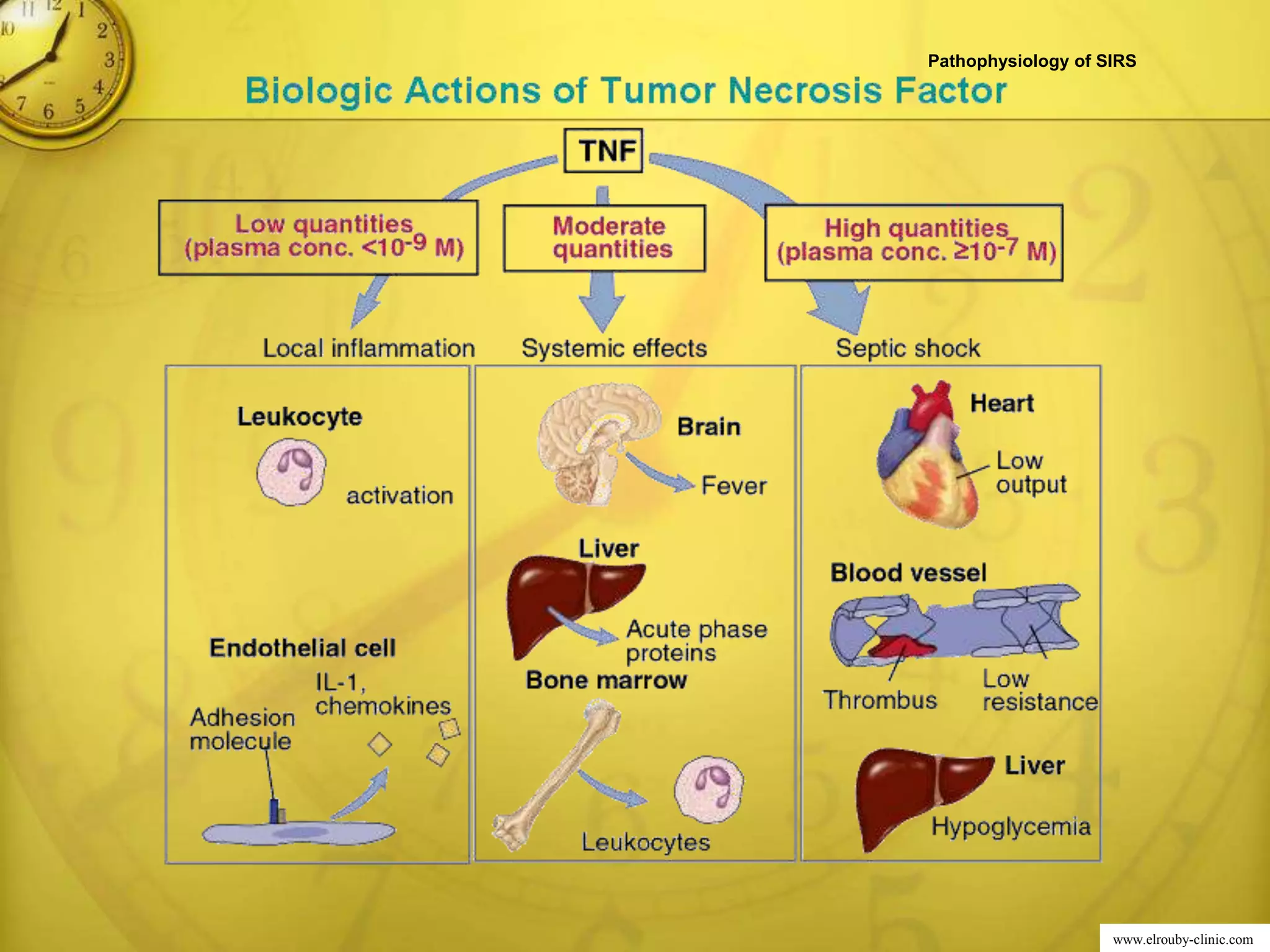
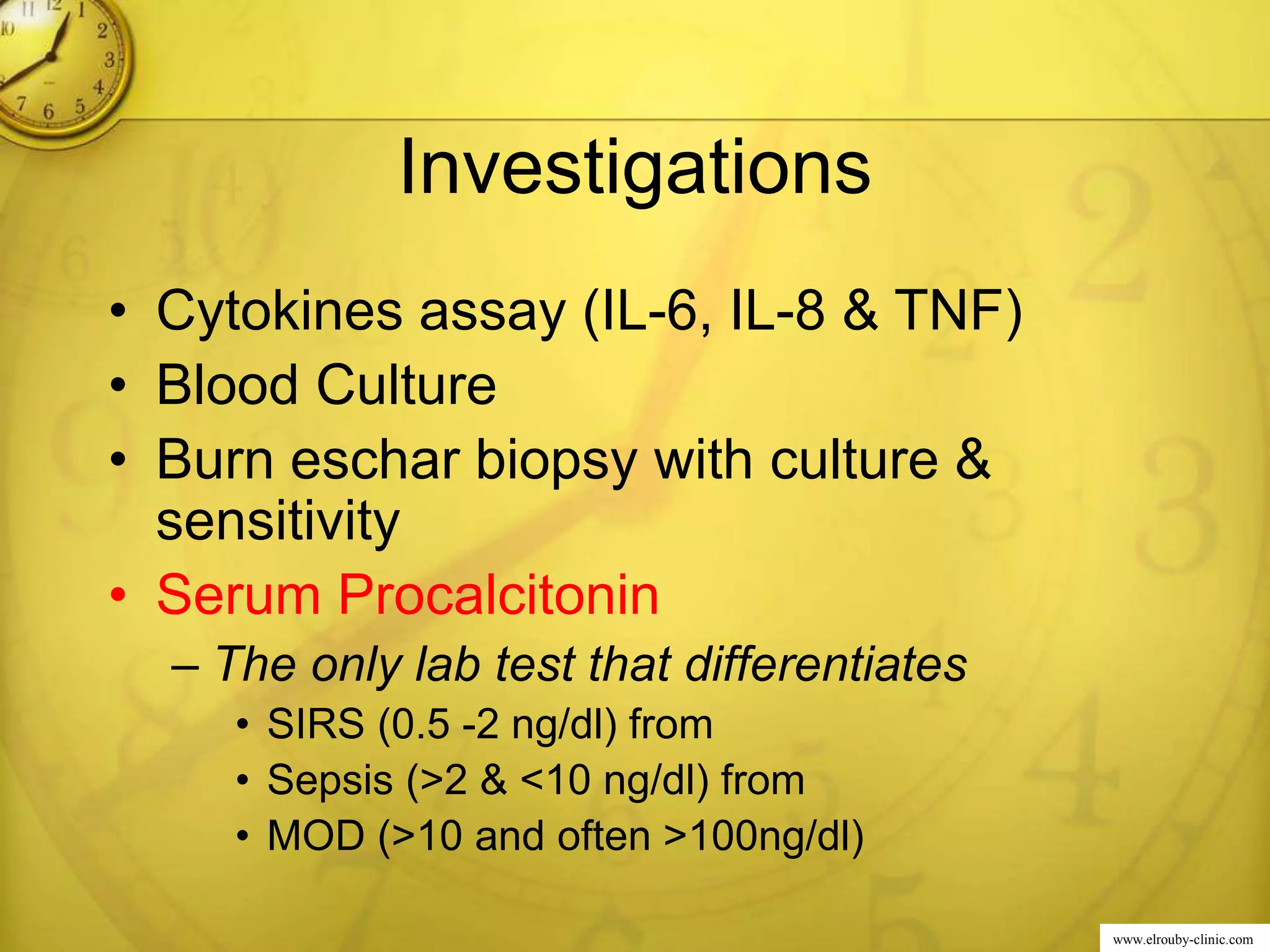
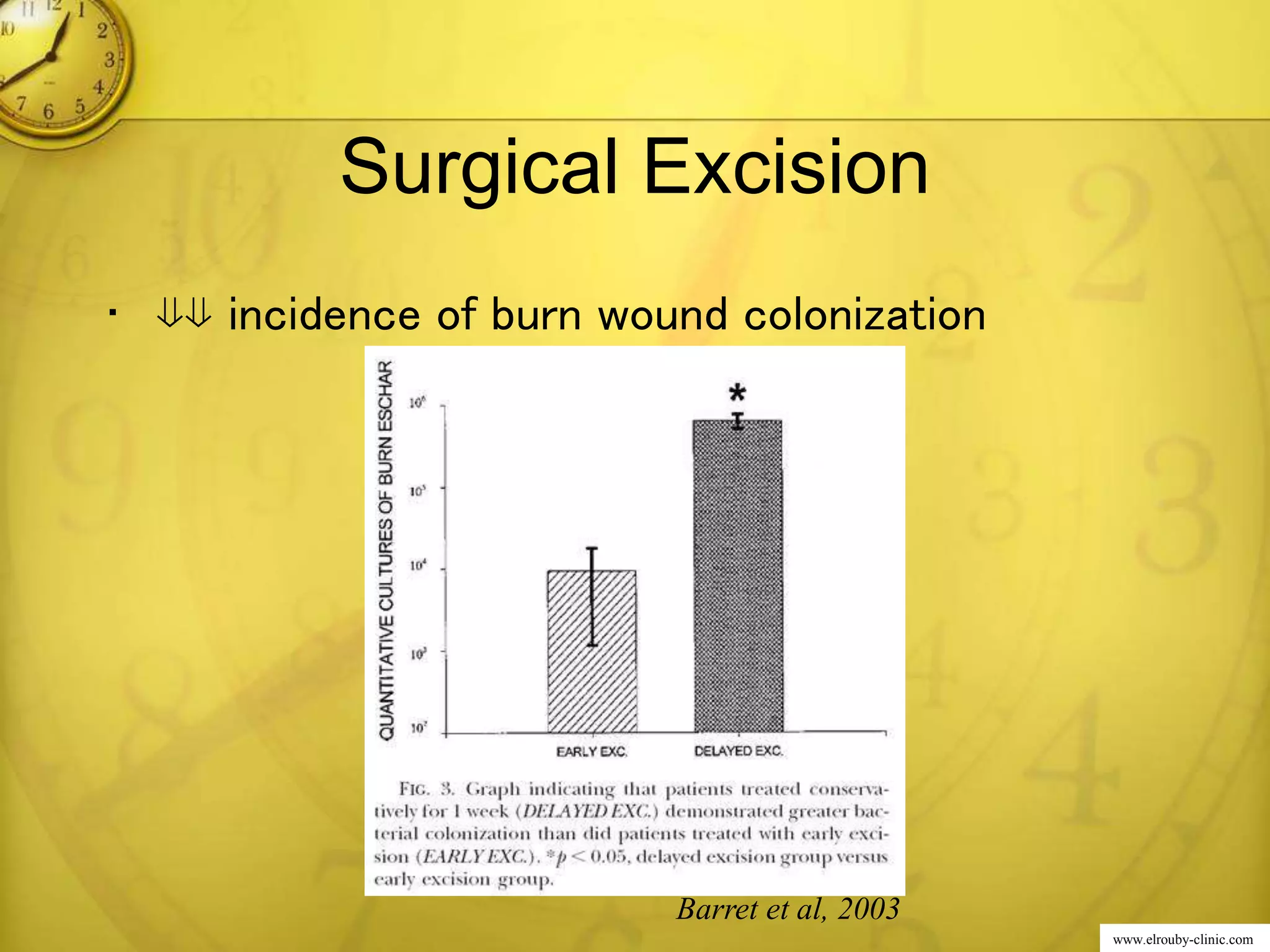
This document provides an overview of systemic inflammatory response syndrome (SIRS) authored by Professor Dr. Mohamed El Rouby. It defines SIRS as a severe systemic response to a critical incidence characterized by disseminated immune activation and capillary dysfunction, which can result in organ dysfunction. The pathophysiology of SIRS involves the release of lipopolysaccharides and lipid-protein complexes from infected or burned tissues, triggering cytokine cascades and immune responses that can lead to multiple organ dysfunction syndrome if not controlled. Treatment focuses on eliminating triggers through antibiotics, wound excision, and supporting organ functions through ventilation, fluids, and inotropes.