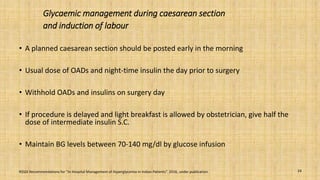
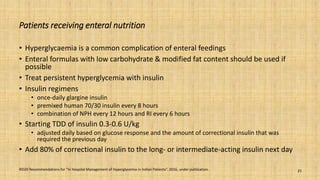
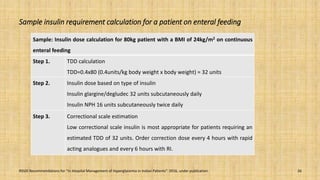
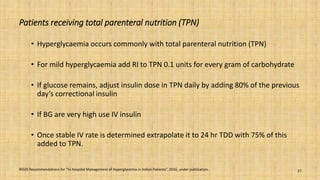
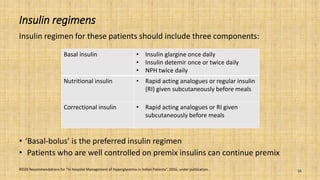
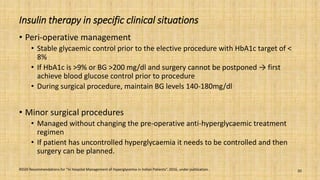
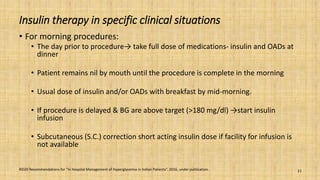
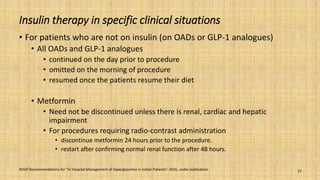
This document provides a comprehensive overview of the management of inpatient hyperglycaemia in non-critically ill patients with type 2 diabetes, highlighting the prevalence of diabetes and hyperglycaemia in hospitalized patients. It discusses glycaemic targets, treatment options such as insulin regimens, and specific clinical situations requiring tailored approaches. The document emphasizes the significance of insulin therapy and presents detailed guidelines for managing hyperglycaemia in various contexts, including surgical procedures and enteral feeding.
![Management of hyperglycaemia during obstetrics
procedures, C-Section and vaginal delivery
• Day care obstetric procedures (cervical cerclage, amniocentesis) do not require more
than 6-8 hours of overnight fasting
• Maintain BG between 70-140 mg/dl during and immediately after the procedure.
Intrapartum glucose management
• Uncontrolled maternal hyperglycaemia during the labour → foetal hyperinsulinism
and neonatal hypoglycaemia
• Maternal BG target during delivery - 70 to 140 mg/dl
• Separate insulin and glucose infusions
• Start insulin infusion at 0.5 -1 U/hr
• 5% Dextrose or dextrose normal saline [DNS] - 80-125 ml/h.
RSSDI Recommendations for “In Hospital Management of Hyperglycemia in Indian Patients”. 2016, under publication. 23](https://image.slidesharecdn.com/inpatienthyperglycemia-190419102435/85/Inpatient-hyperglycemia-ver3-3-23-320.jpg)