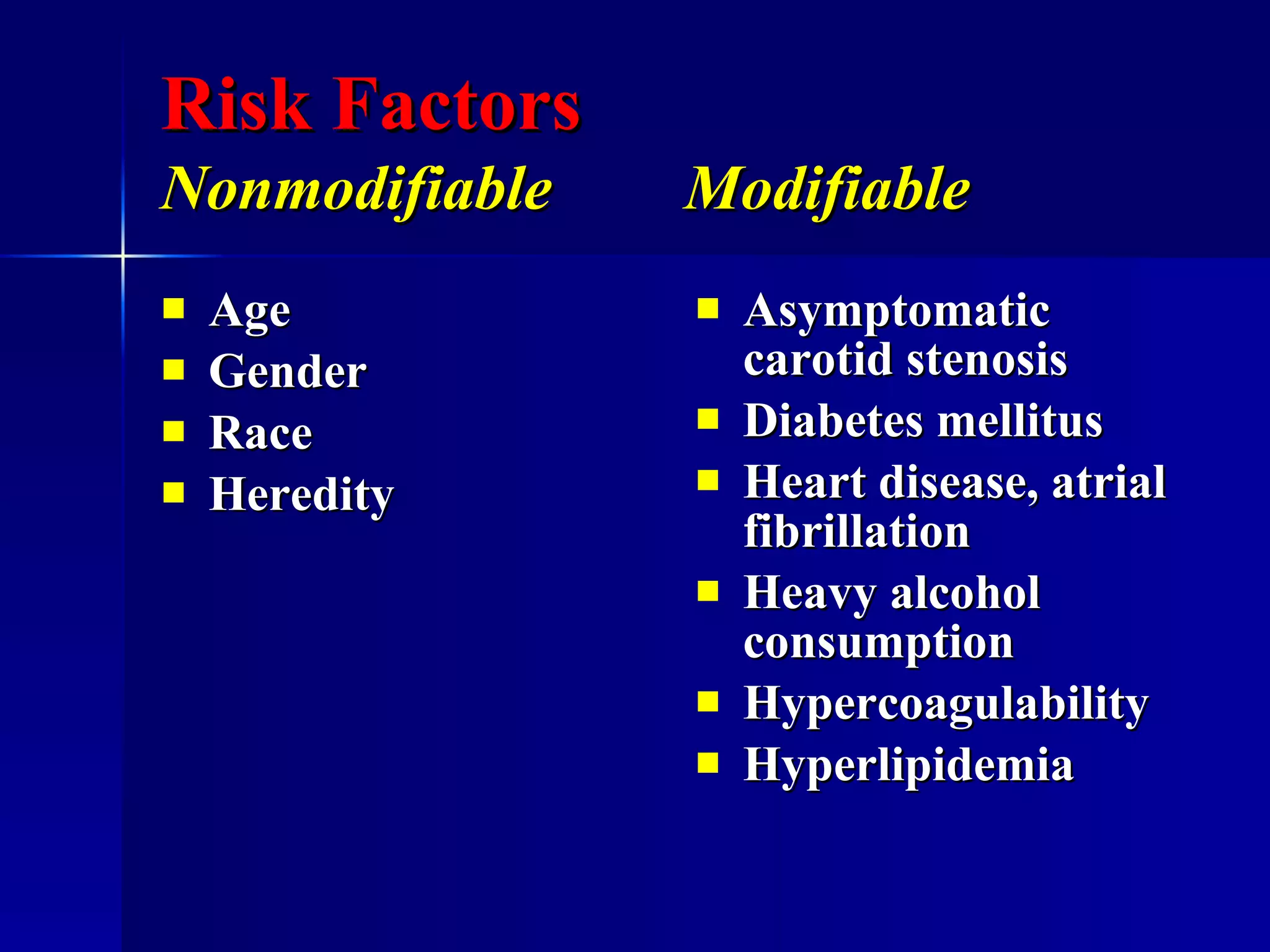
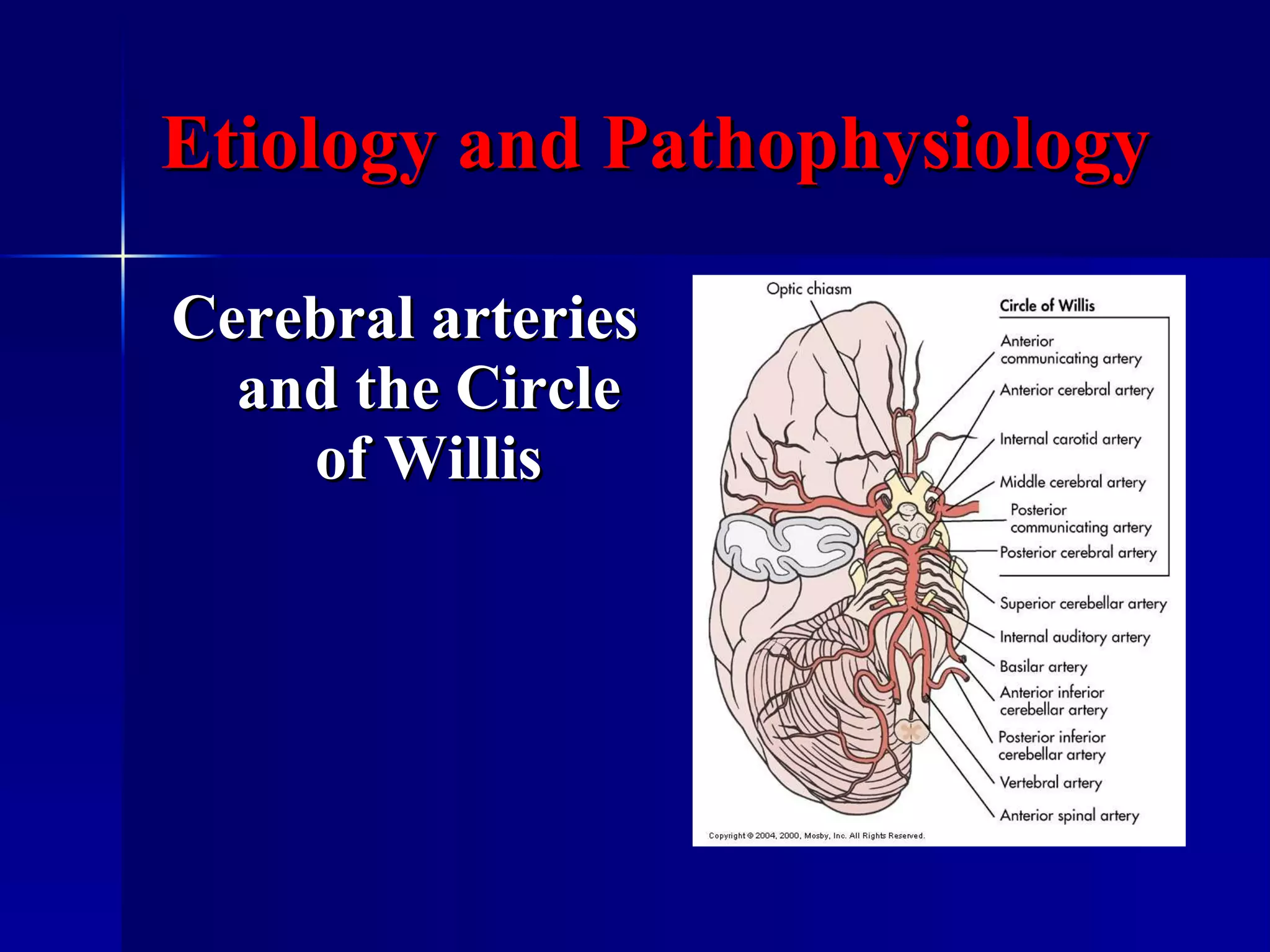
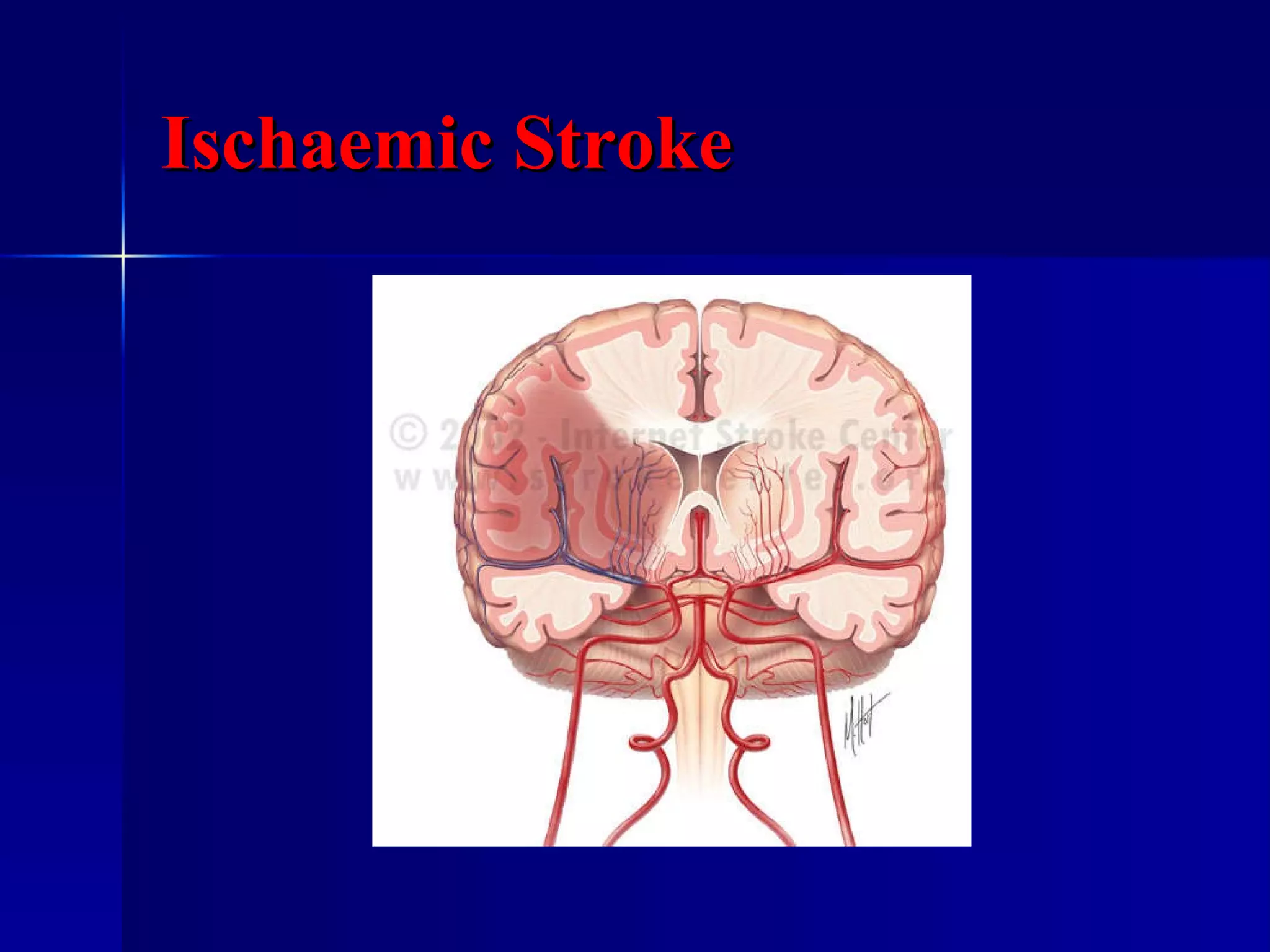
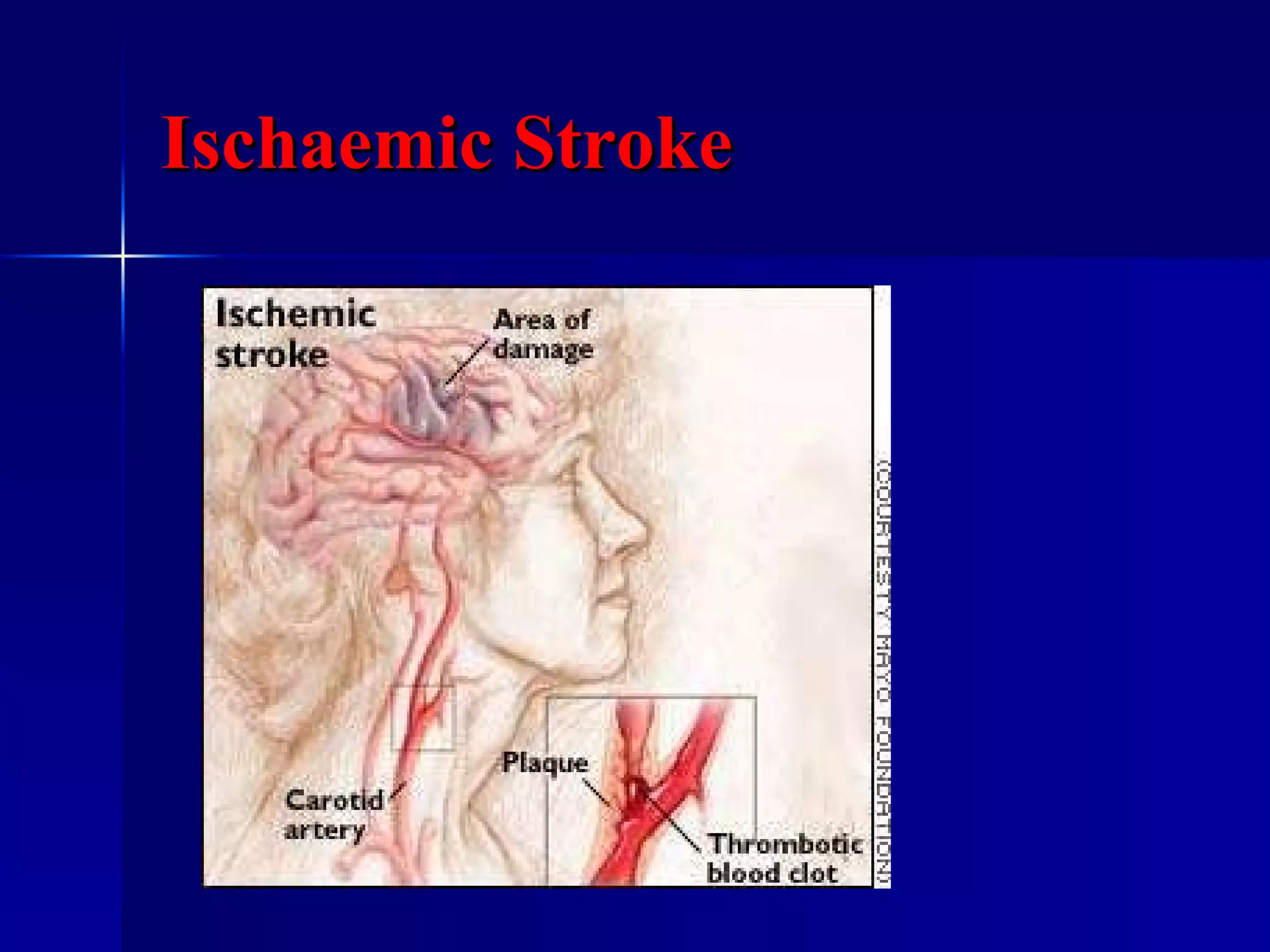
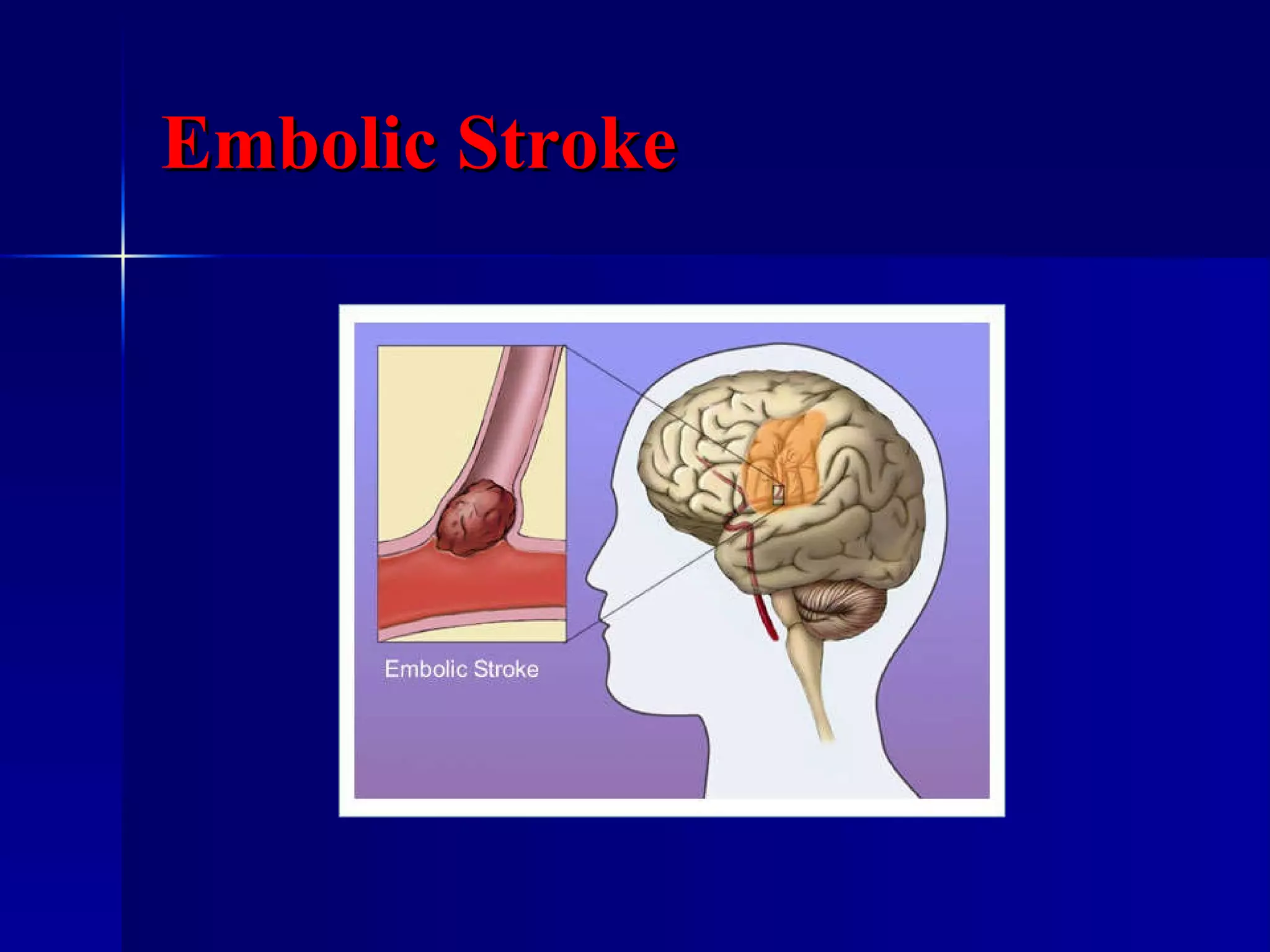
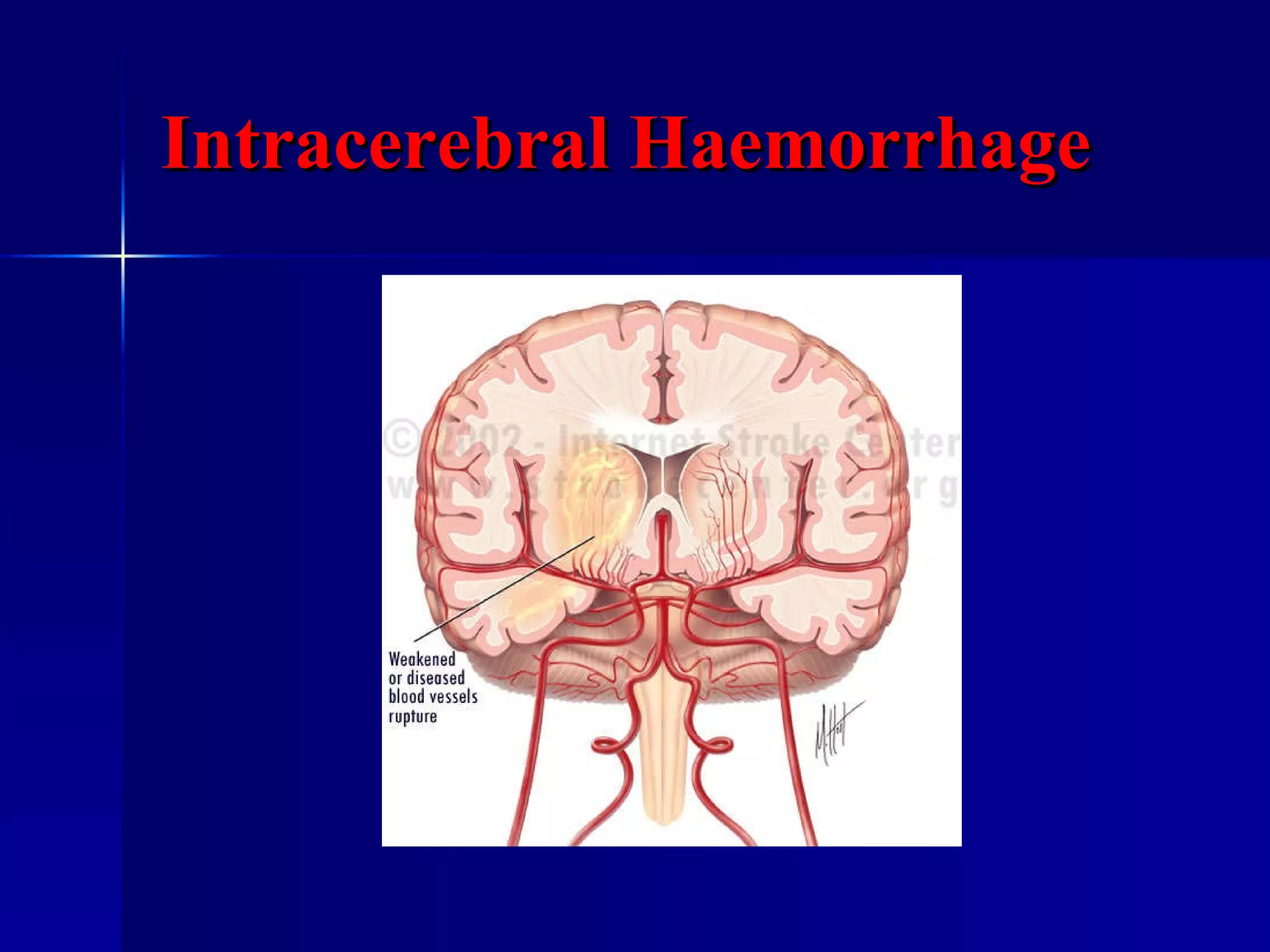
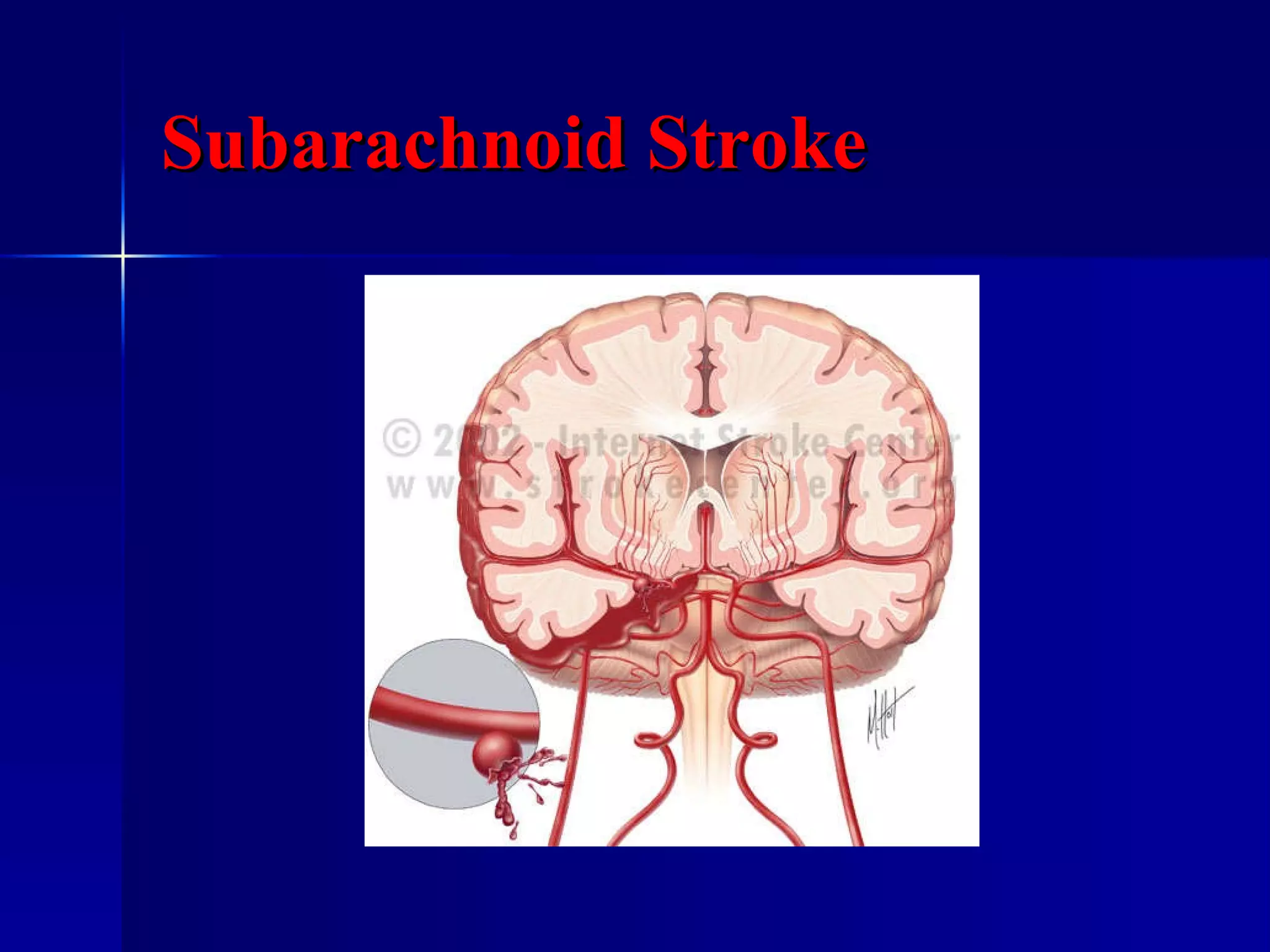
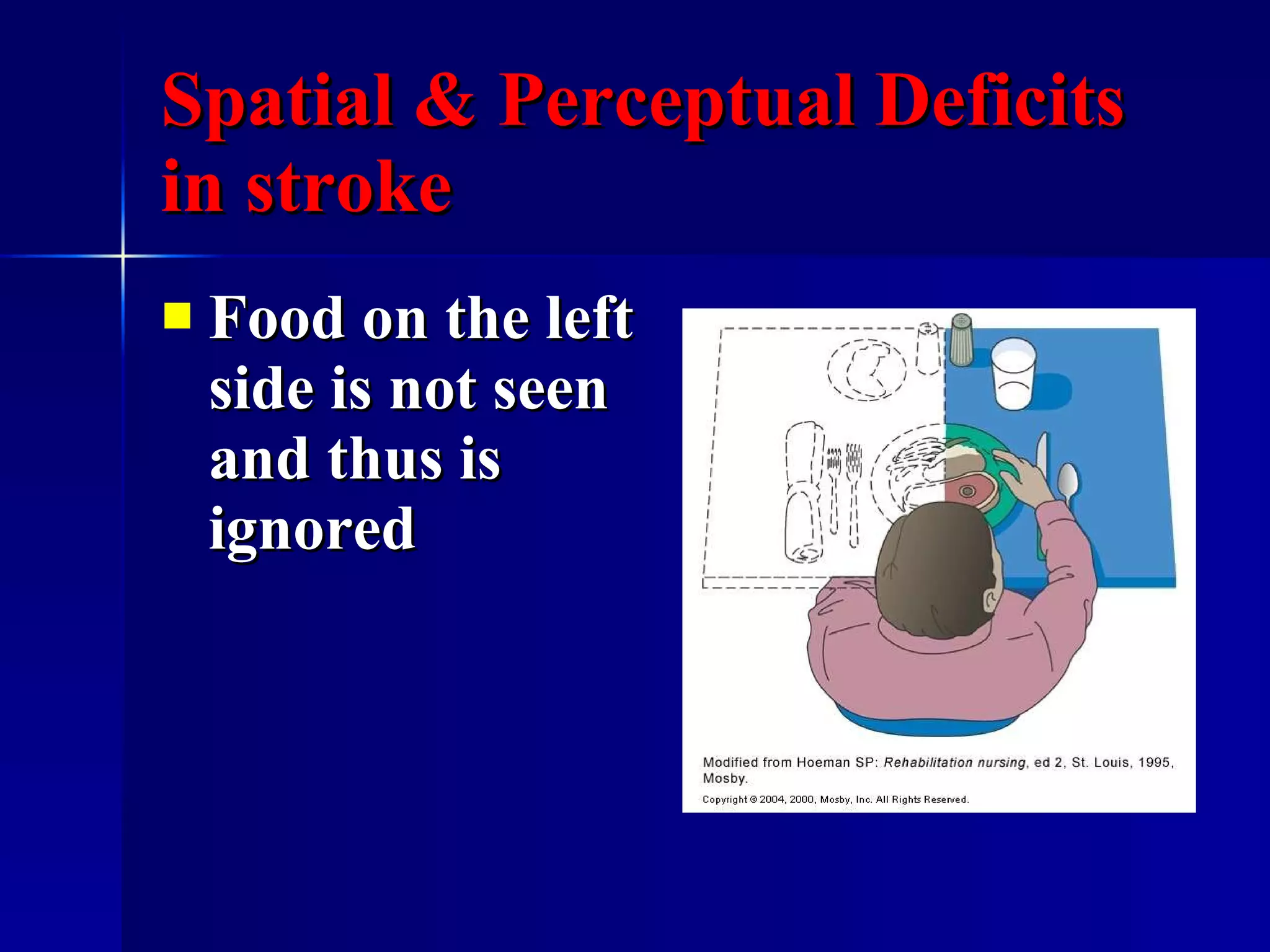
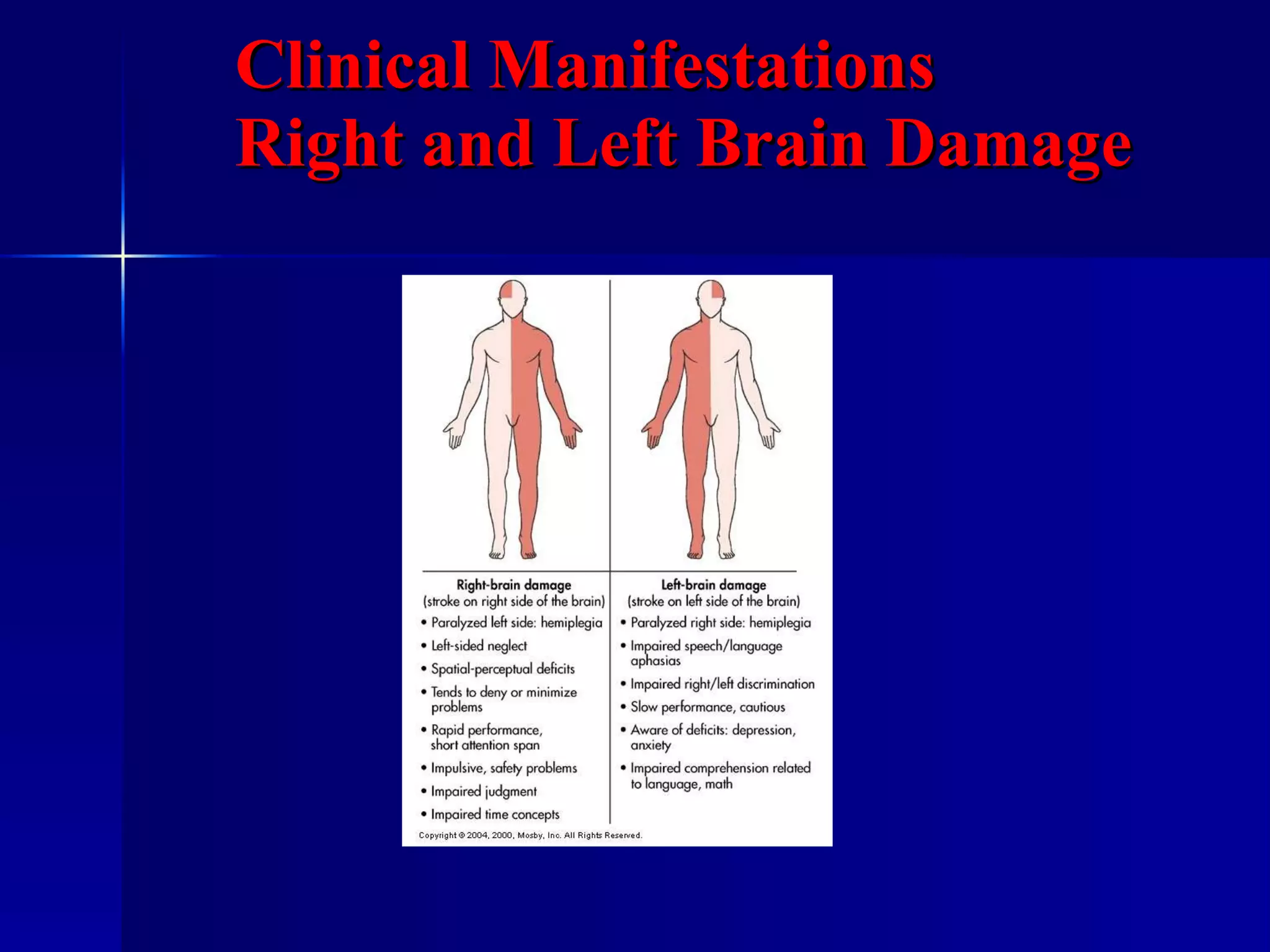
Stroke occurs when there is inadequate blood flow to the brain resulting in cell death. It is a leading cause of death and disability. There are two main types - ischemic caused by clots or blockages cutting off blood flow, and hemorrhagic caused by bleeding within or around the brain. Strokes cause deficits varying by location but often involve motor, communication, cognitive and emotional impairments. Risk factors include hypertension, smoking, obesity, age, and heredity.