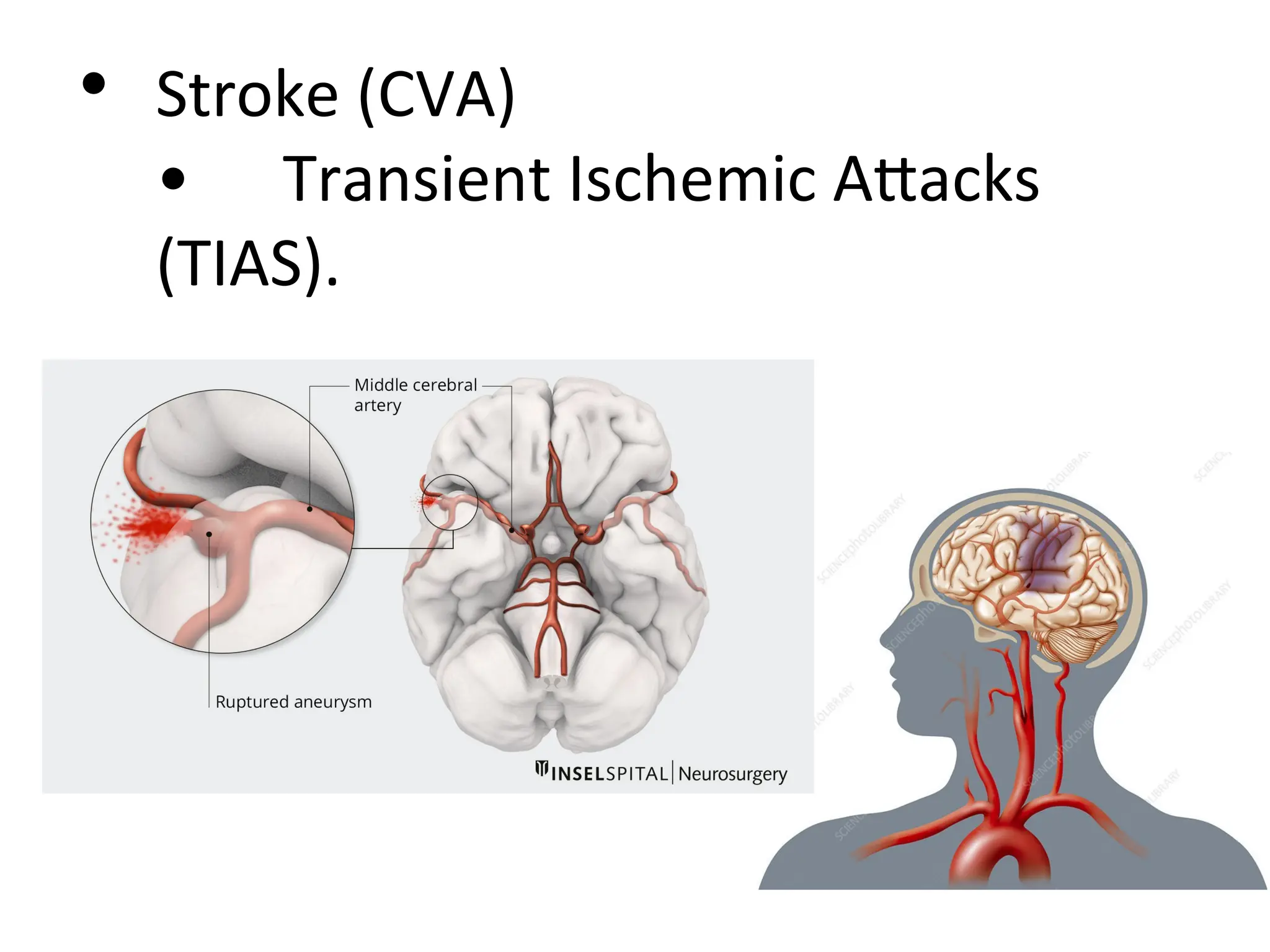
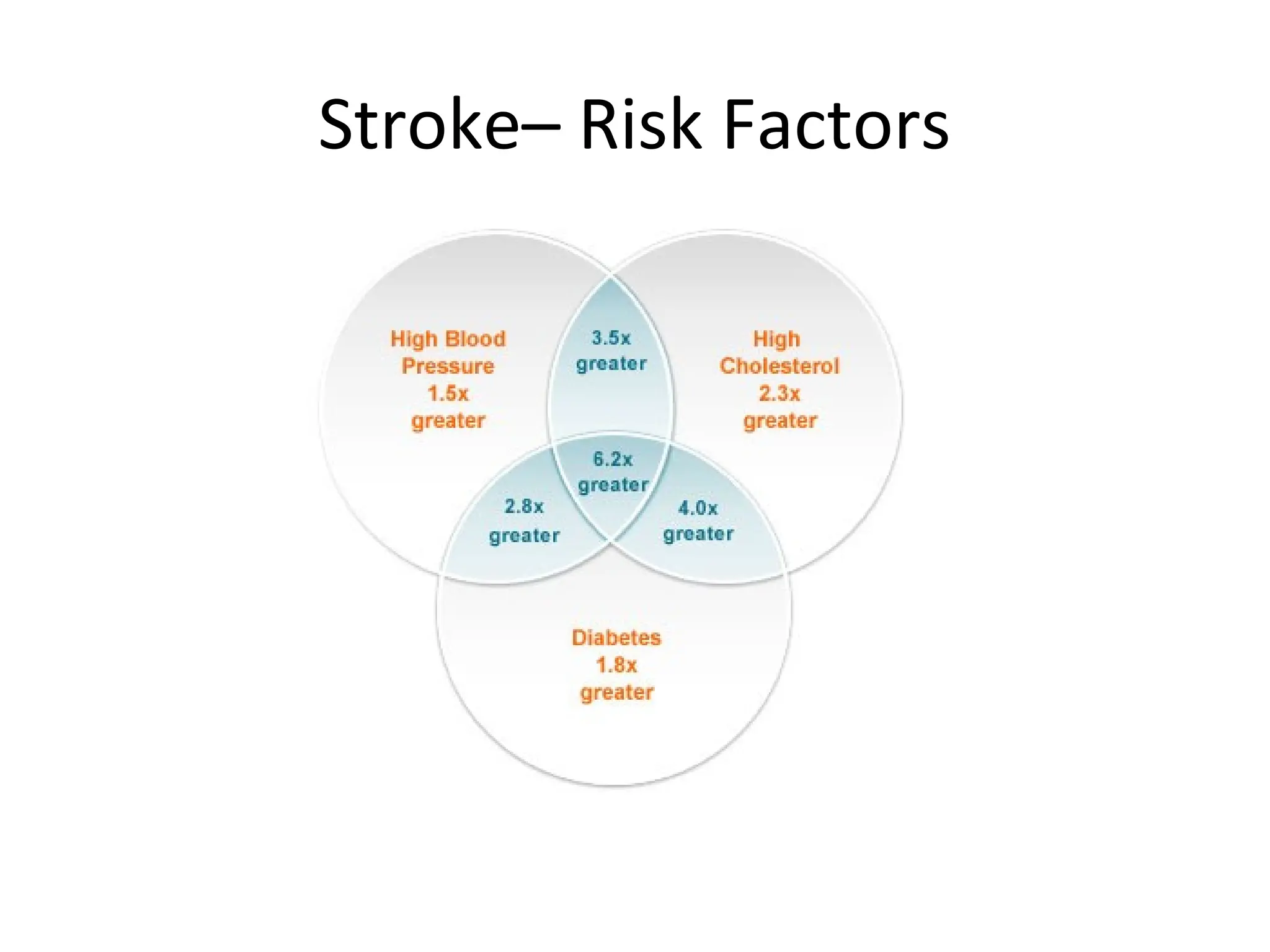
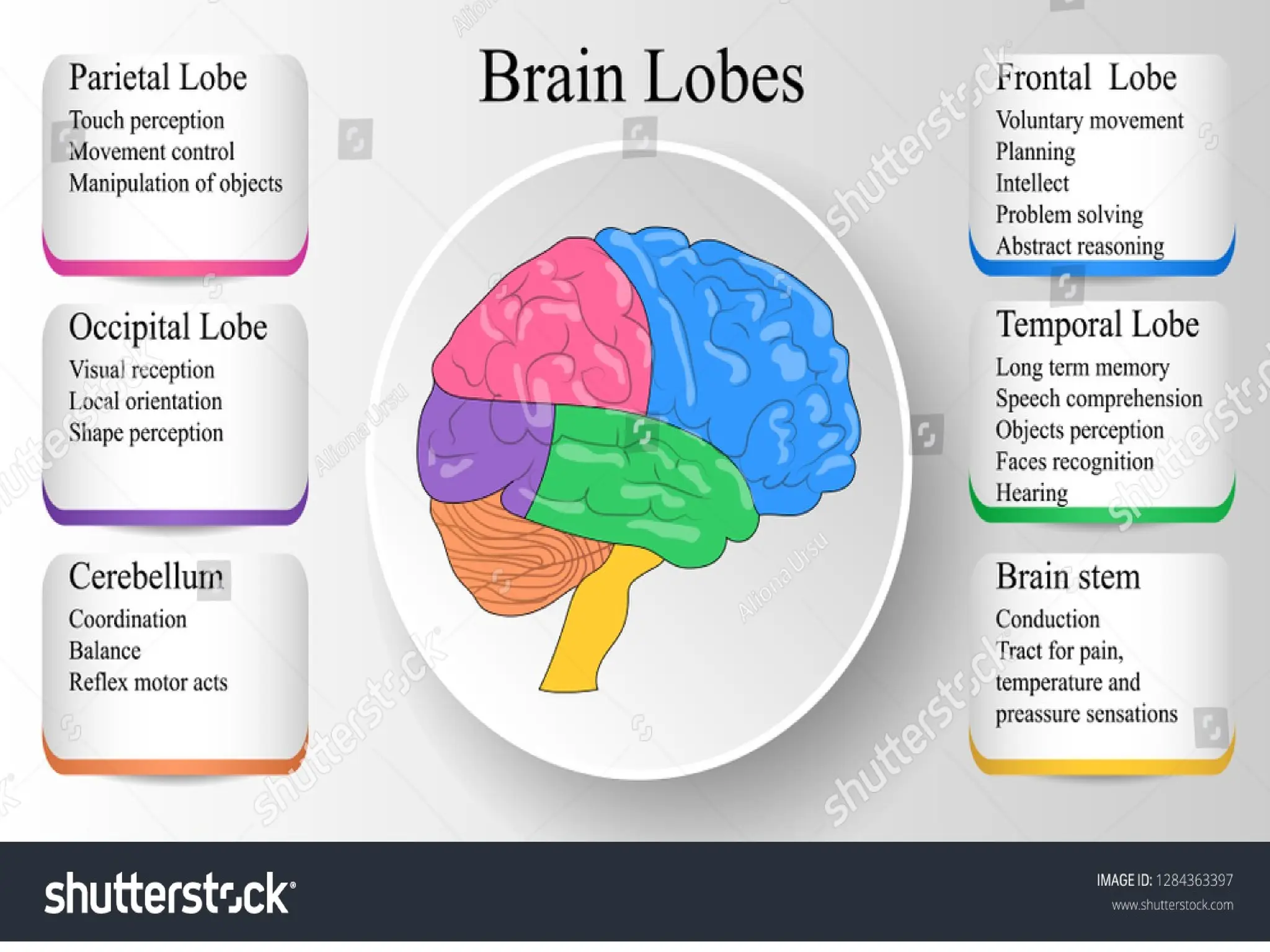
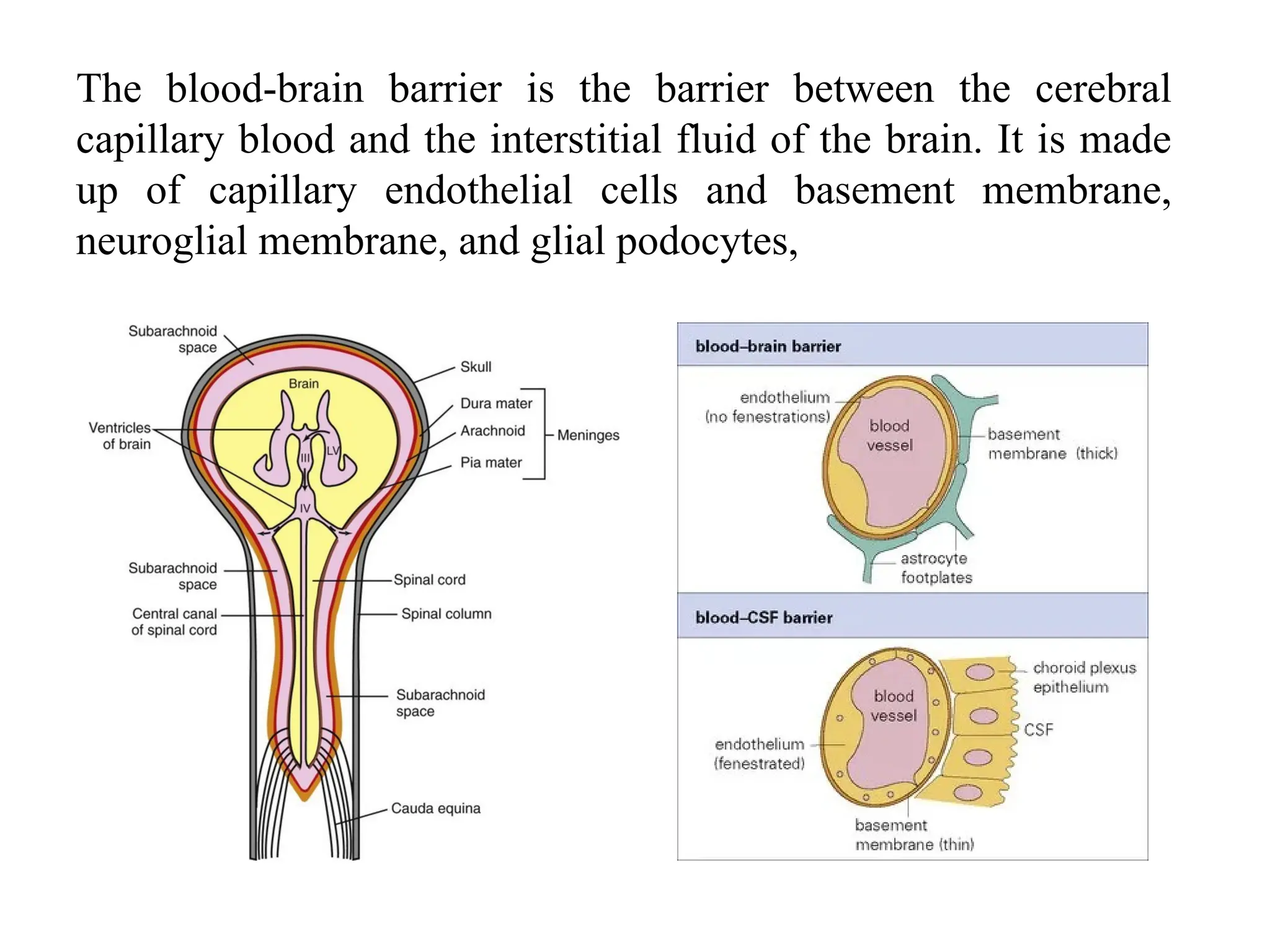
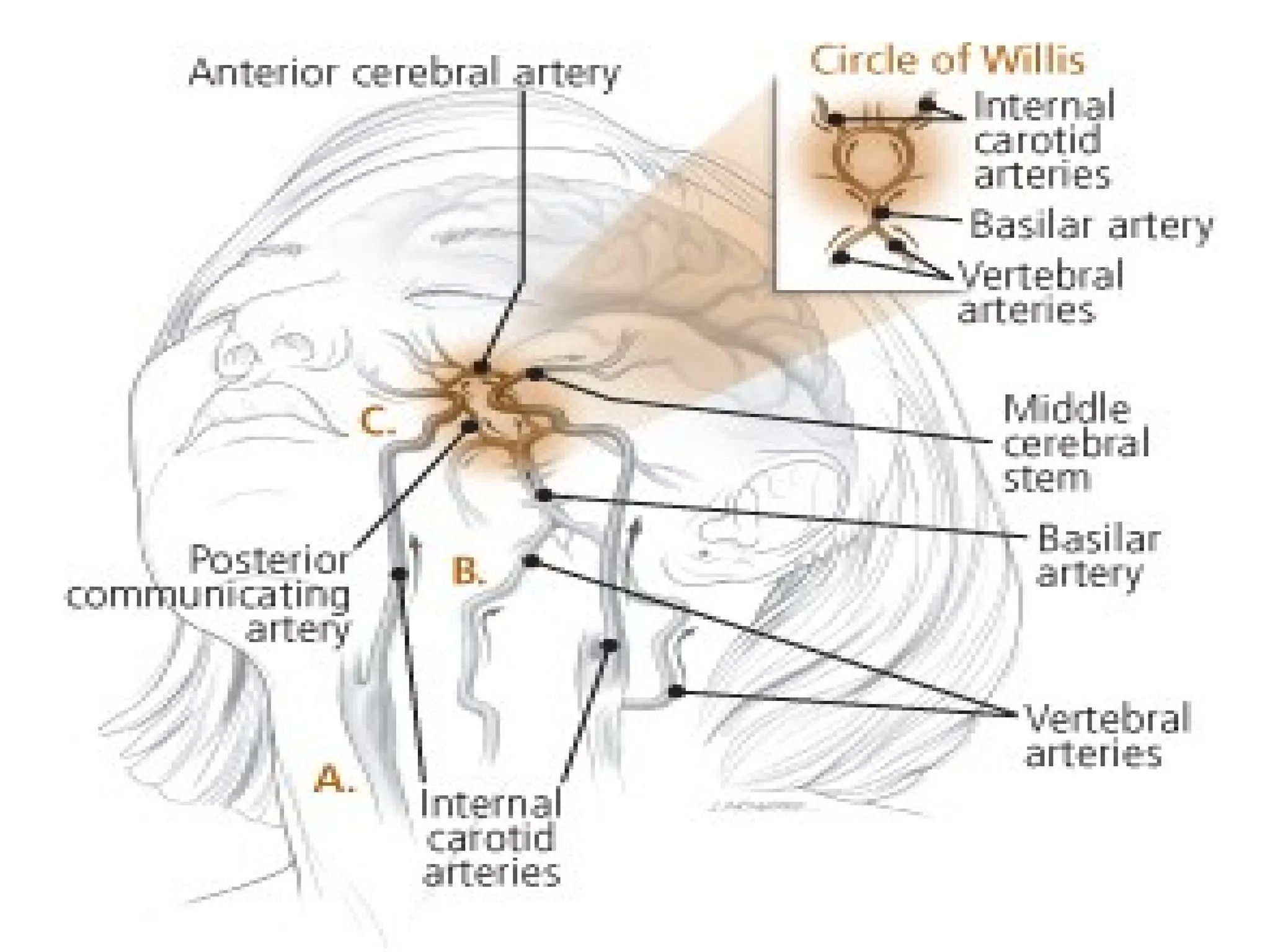
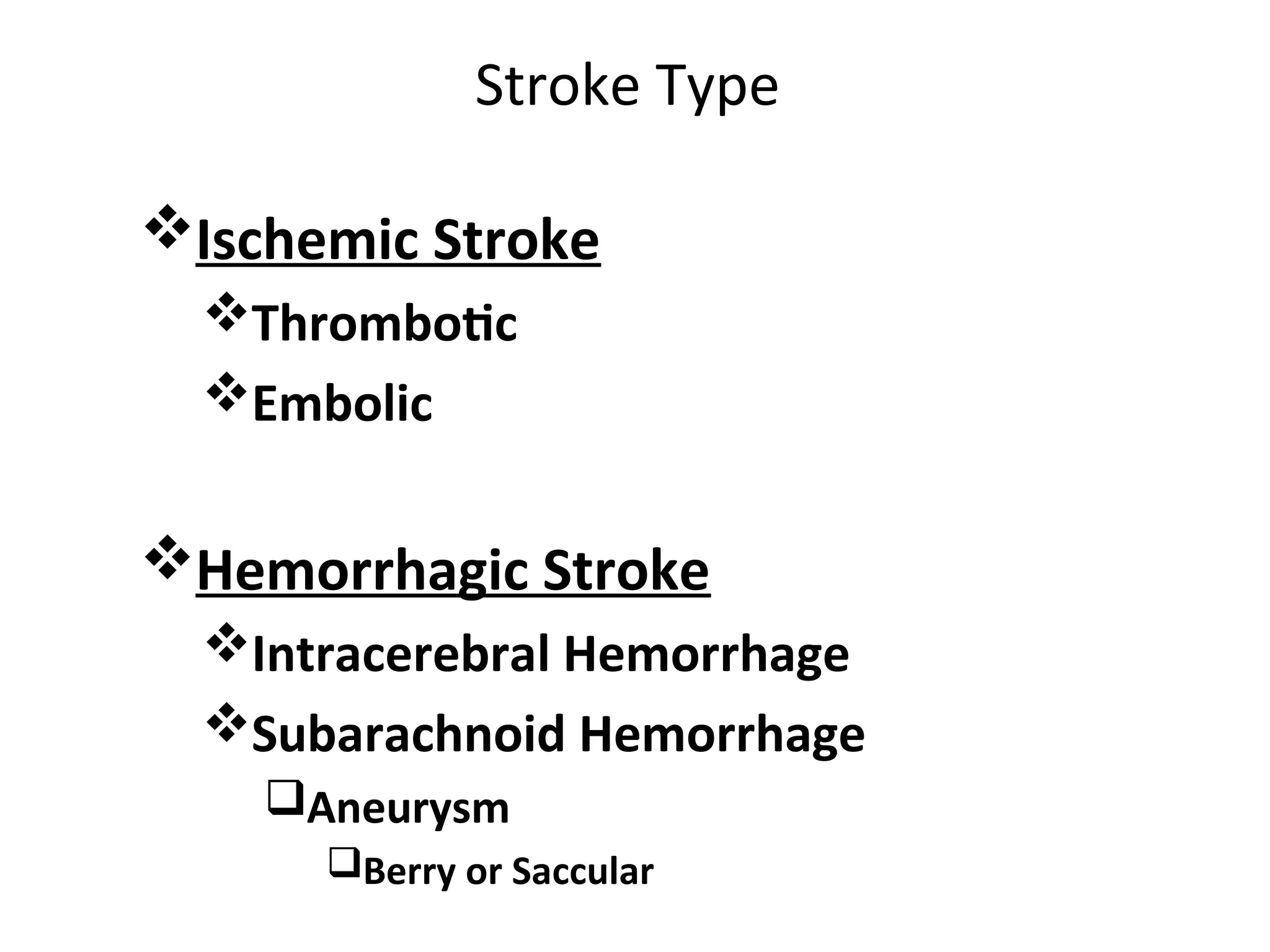
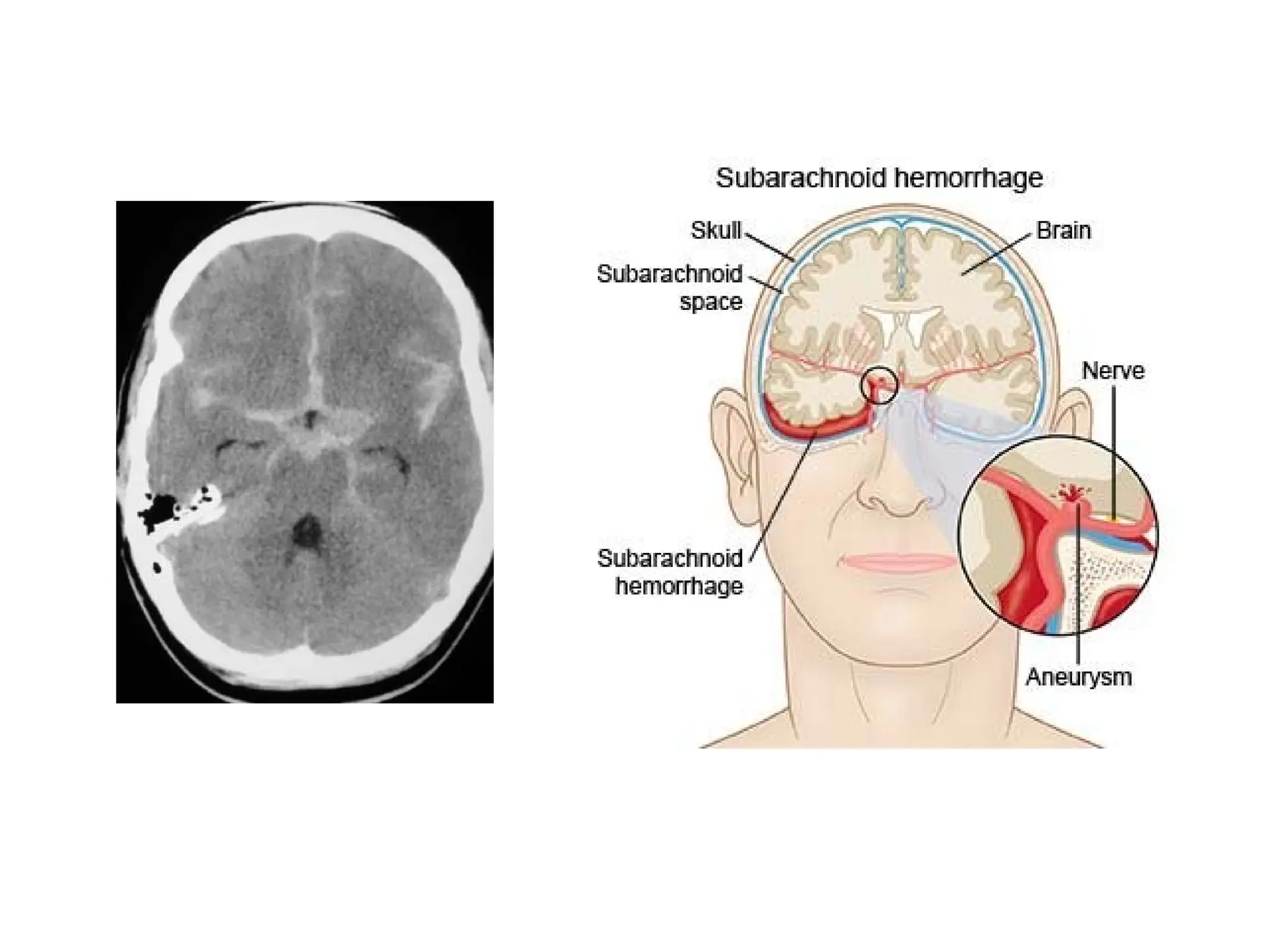
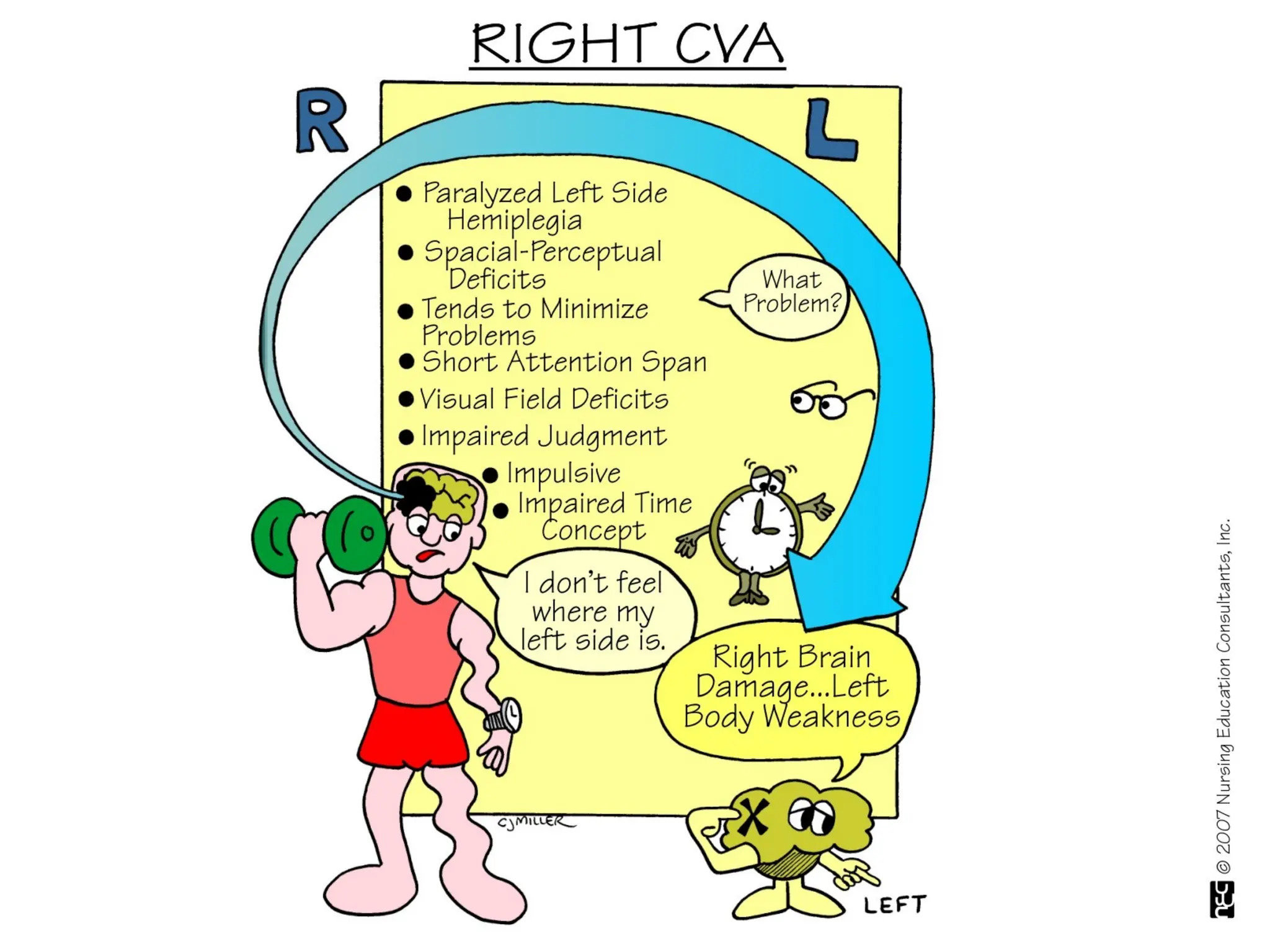
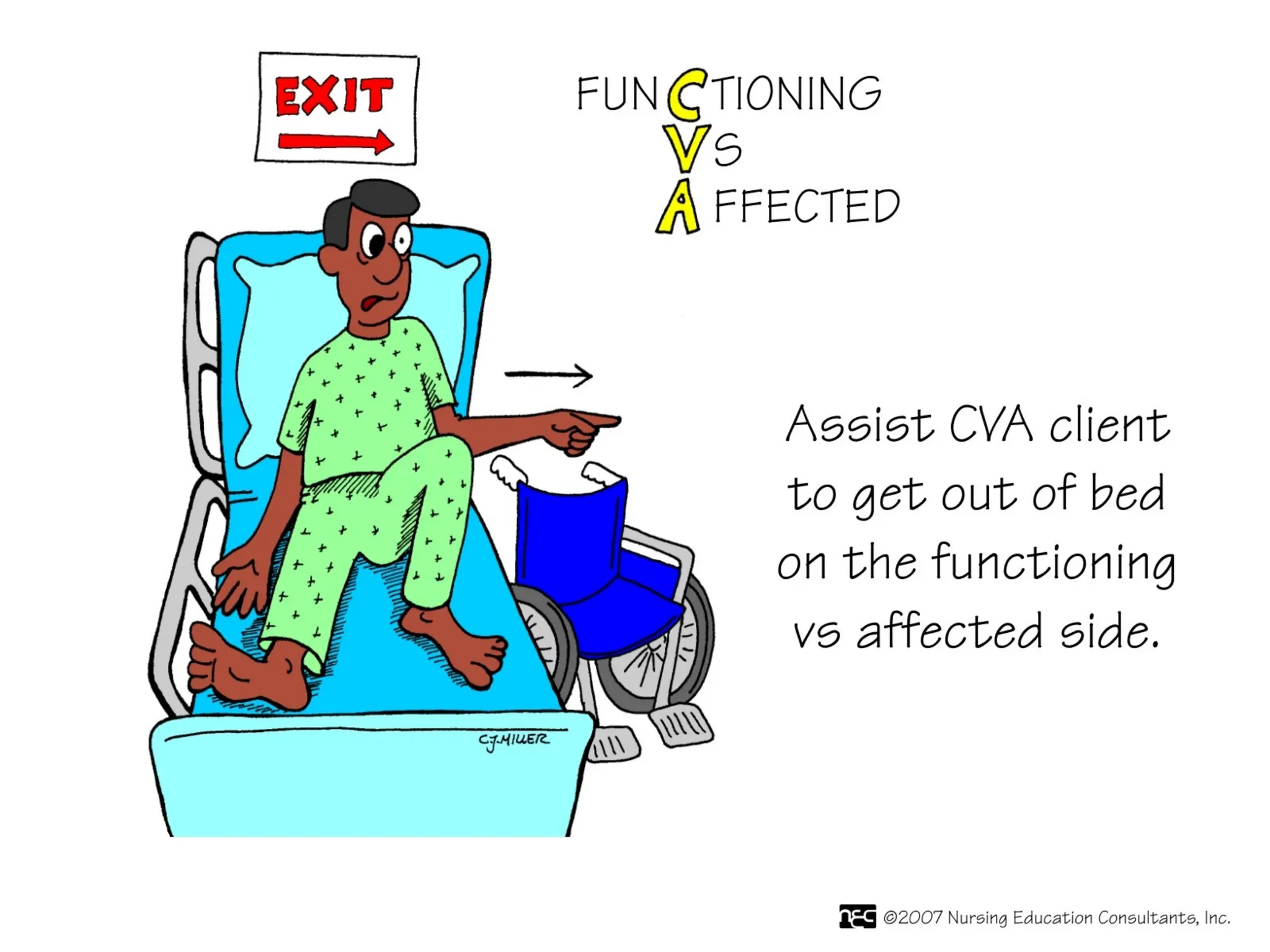
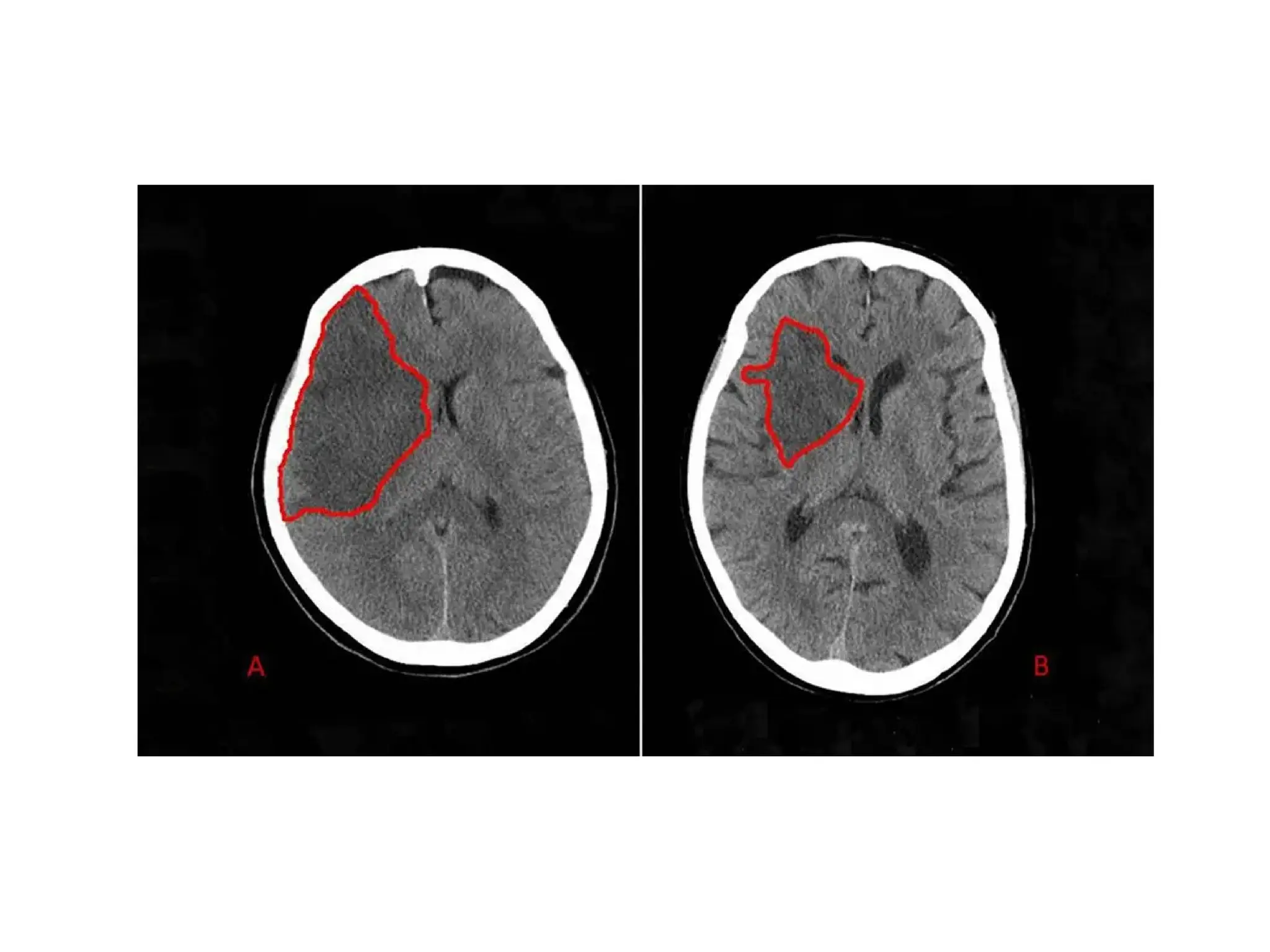
The document provides an overview of neurological disorders, specifically focusing on strokes and transient ischemic attacks (TIAs). It outlines the anatomy of cerebral circulation, types of strokes (ischemic and hemorrhagic), their risk factors, pathophysiology, and clinical manifestations. Furthermore, it emphasizes the importance of prevention, early treatment, and rehabilitation to manage the effects of strokes.