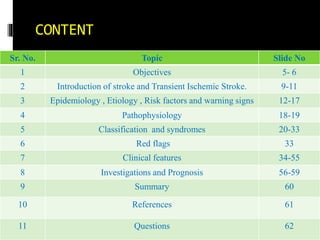
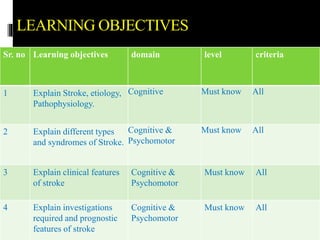
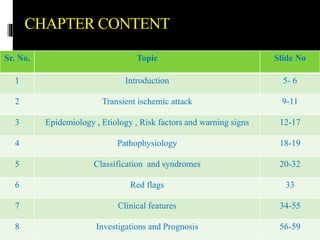
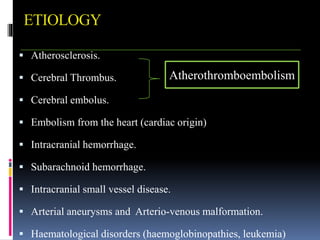
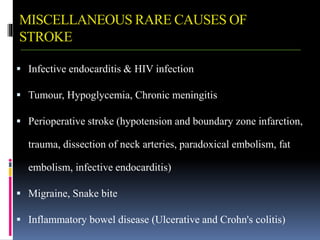
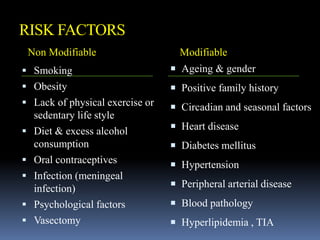
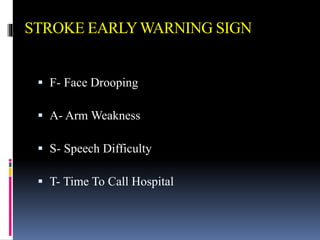
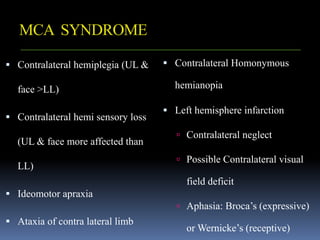
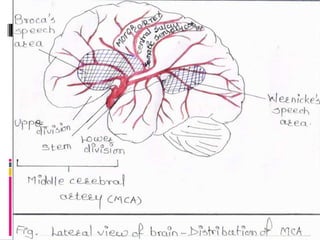
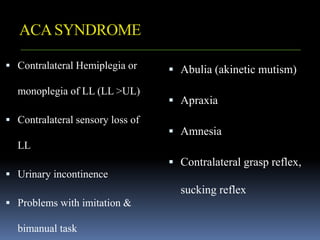
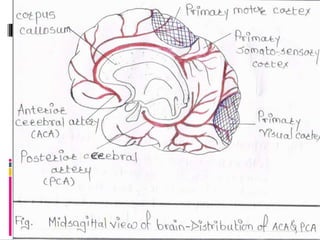
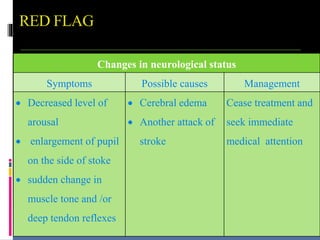
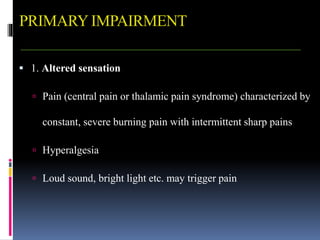
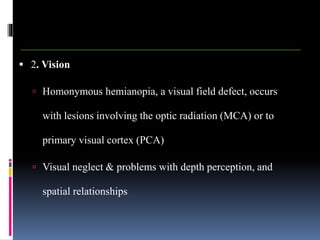
This document is a comprehensive presentation on strokes, covering their introduction, classification, epidemiology, etiology, risk factors, pathophysiology, clinical features, investigations, and prognosis, aimed primarily at final year bachelor of physiotherapy students. Key learning objectives include understanding stroke definitions, causes, syndromes, clinical features, and the necessary investigations. It also discusses the various types, symptoms, and recovery related to strokes, along with references and questions for further assessment.