This document provides information about strokes, including:
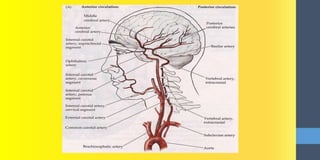
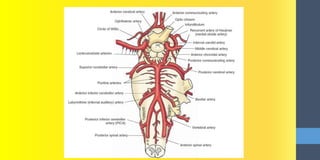
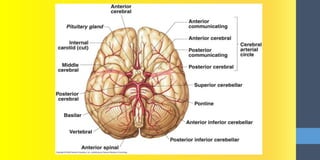
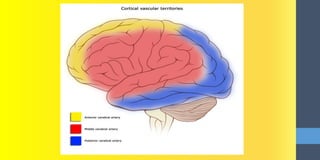
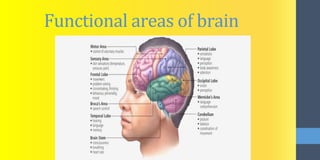
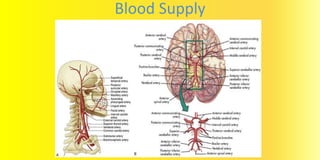
- The anatomy of the brain and its blood supply from arteries.
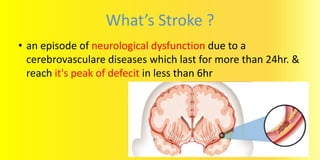
- The definition of a stroke as a neurological dysfunction lasting over 24 hours due to cerebrovascular disease.
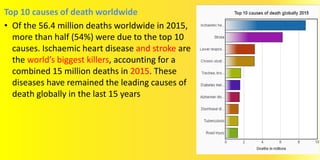
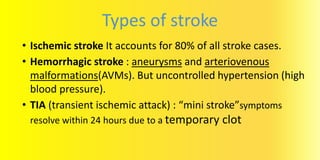
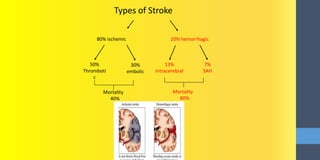
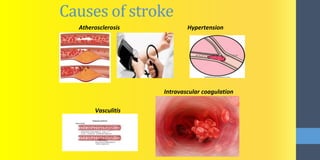
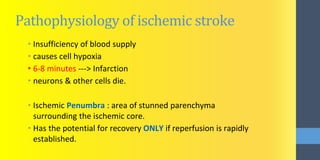
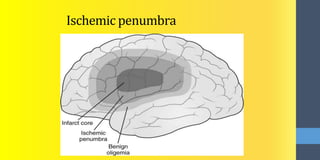
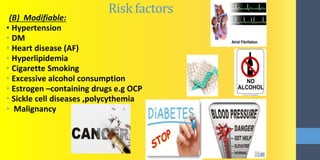
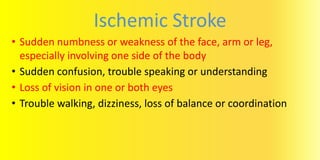
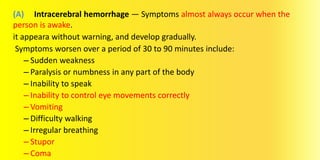
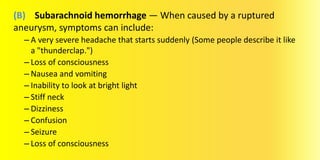
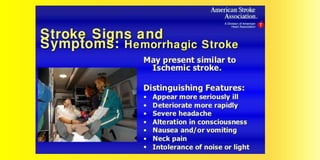
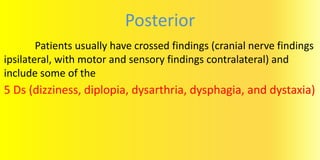
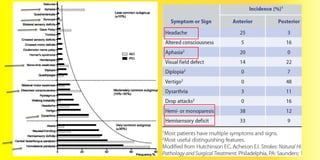
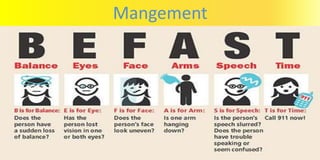
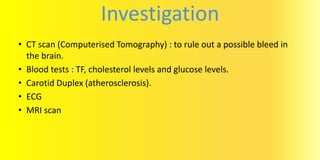
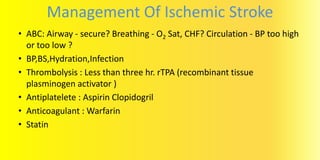
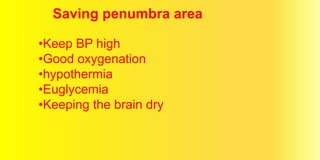
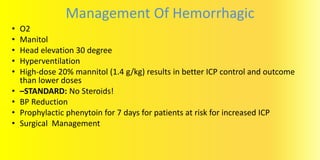
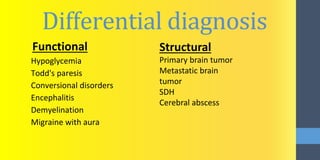
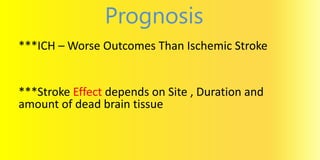
- The types, causes, risk factors, signs and symptoms, and management of ischemic and hemorrhagic strokes.
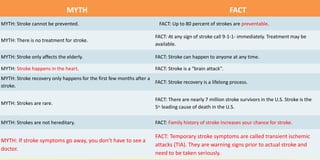
- Myths and facts about strokes, including that up to 80% are preventable but they can affect anyone at any time.
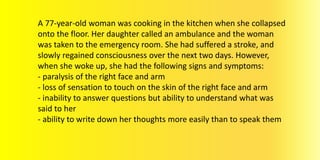
It then discusses the case of a 77-year-old woman who suffered paralysis on her right side and an inability to speak after a stroke, indicating a left middle cerebral artery blockage.