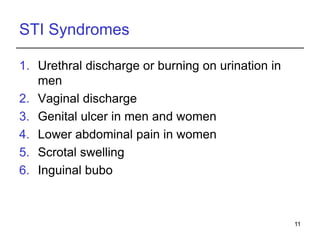
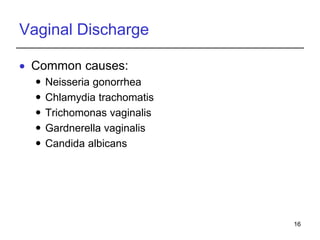
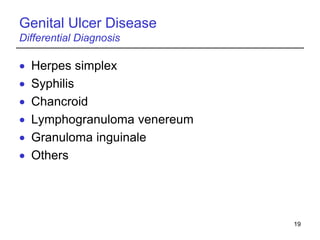
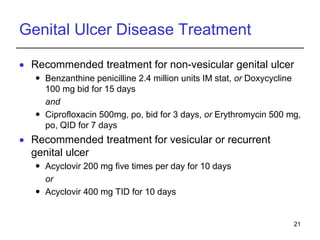
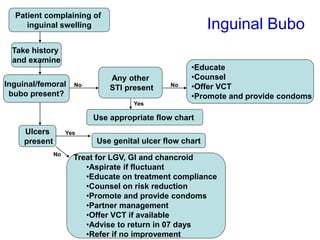
This document discusses sexually transmitted infections (STIs) and provides information on commonly encountered STIs, their symptoms, treatments, and links to HIV transmission. It describes how STIs like chlamydia, gonorrhea, and syphilis can increase the risk of HIV transmission by 2 to 9 times. The document outlines syndromic approaches and recommended treatments for various STI syndromes like urethral discharge, vaginal discharge, genital ulcers, lower abdominal pain, scrotal swelling, inguinal bubo, and neonatal conjunctivitis. It emphasizes that STIs and HIV infection often affect the same populations and share similar risk factors.