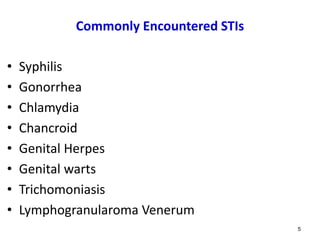
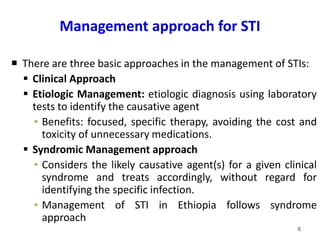
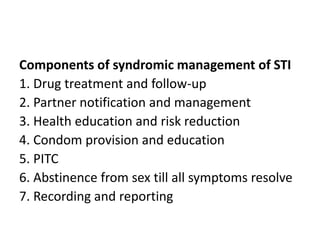
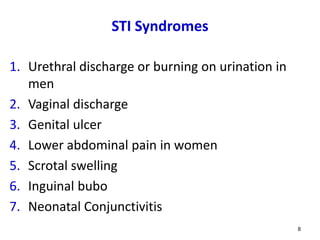
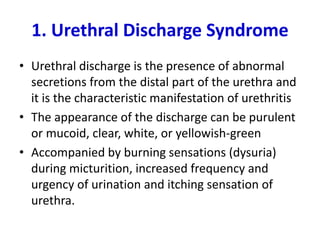
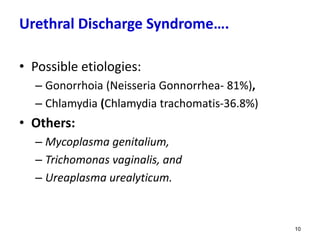
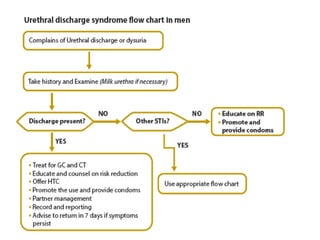
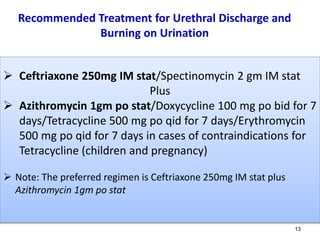
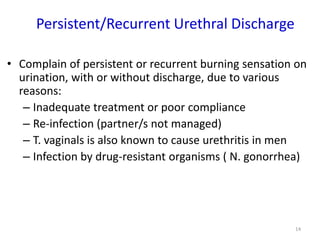
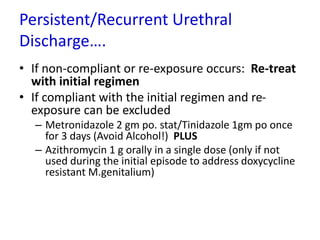
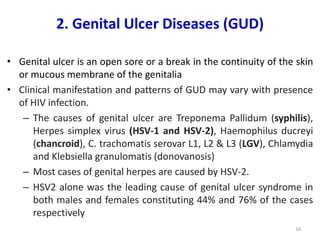
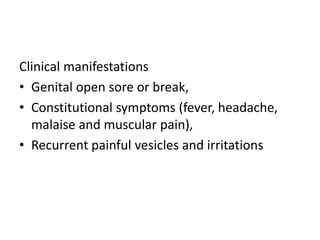
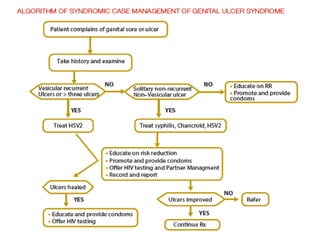
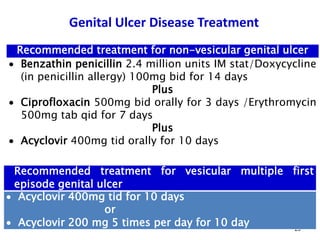
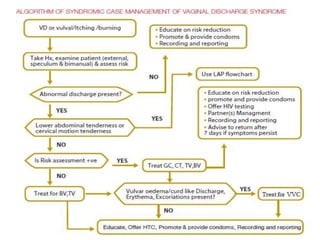
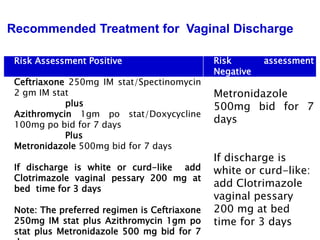
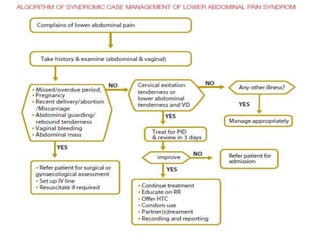
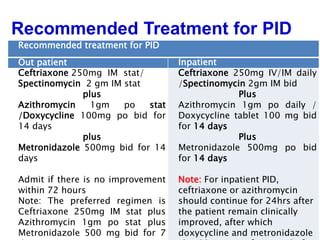
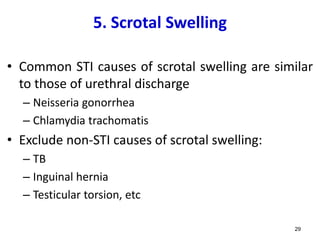
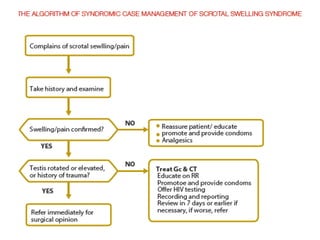
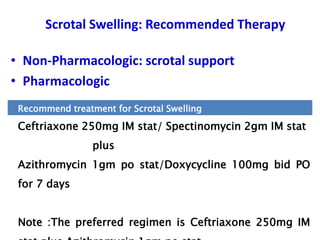
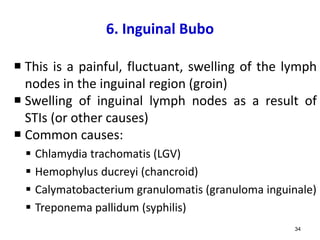
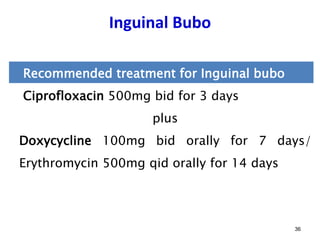
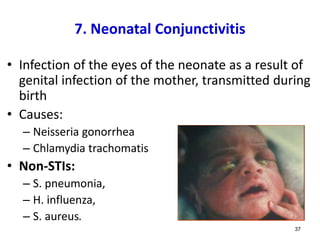
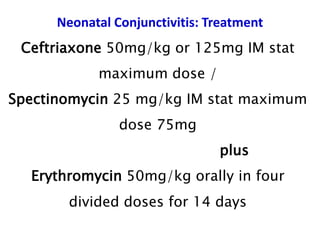
The document discusses sexually transmitted infections (STIs), describing their causes, symptoms, modes of transmission and effective treatment approaches. It focuses on commonly encountered STIs like syphilis, gonorrhea, chlamydia, herpes, and HIV. Management of STIs is outlined according to syndrome-based approaches like urethral discharge, genital ulcers, vaginal discharge, lower abdominal pain, and neonatal conjunctivitis.