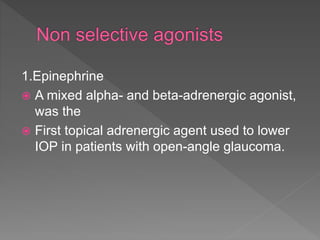
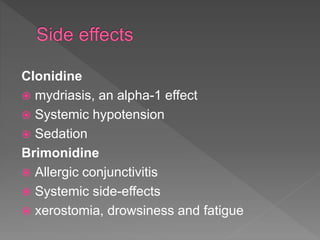
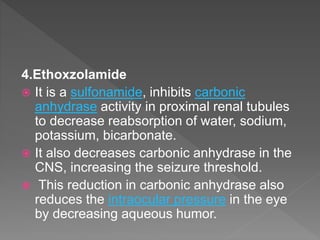
Aqueous humor is formed by the ciliary processes and flows from the posterior to anterior chamber, exiting through the trabecular and uveoscleral routes. It is continuously formed and drained at a rate of approximately 2.5mL/min. Aqueous outflow occurs through pressure-dependent (trabecular) and pressure-independent (uveoscleral) pathways. Various receptors and drugs that act on these pathways to regulate intraocular pressure are discussed. Common glaucoma medications include prostaglandin analogs, beta-blockers, alpha agonists, cholinergic agonists, and carbonic anhydrase inhibitors.