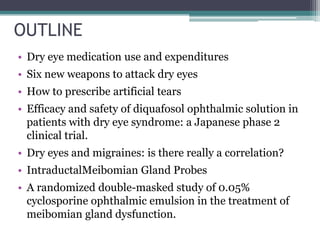
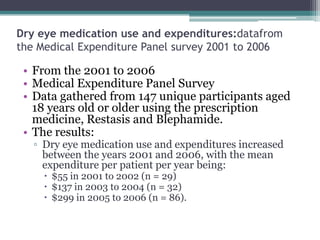
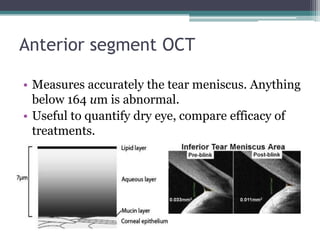
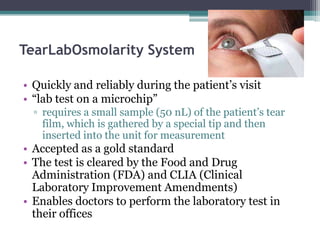
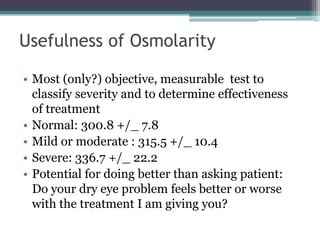
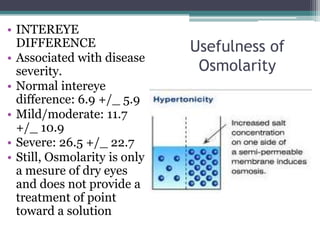
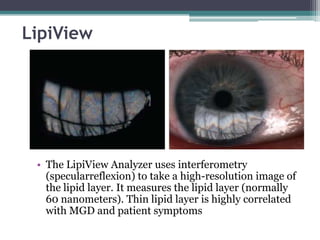
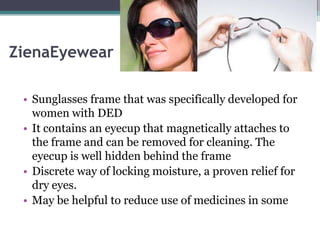
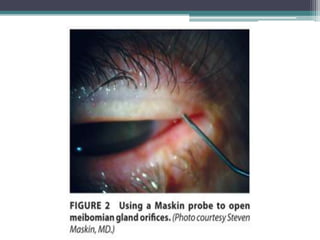
This document outlines several new treatments and technologies for dry eye disease. It discusses increased expenditures on dry eye medications from 2001-2006 driven by Restasis. Six new tools to treat dry eyes are described, including anterior segment OCT, osmolarity testing, LipiFlow, Inflammadry, Ziena eyewear, and intraductal meibomian gland probes. New artificial tear formulations and the use of diquafosol and cyclosporine for dry eyes are also covered.