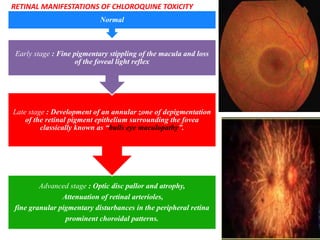
This presentation emphasizes the importance of screening for chloroquine retinopathy according to new AAO guidelines. While bull's eye maculopathy is a classic late-stage sign, initial photoreceptor damage typically occurs parafoveally in Europeans and peripherally near the arcades in Asians. Screening tests like automated visual fields and SD-OCT can detect toxicity before visible RPE damage, as irreversible progression often occurs by the time bull's eye maculopathy appears. Risk of toxicity depends on daily dose, with very thin patients at increased risk when dose is based on ideal rather than actual weight.