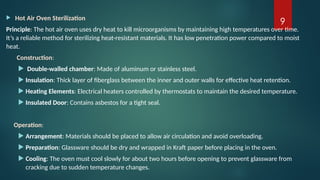
The document provides an extensive overview of various sterilization methods essential for ensuring that medical and laboratory products are free from harmful microorganisms. It categorizes sterilization techniques into physical methods (e.g., dry heat, moist heat, radiation, filtration) and chemical methods (e.g., gaseous sterilization), detailing their mechanisms, applications, and limitations. The document emphasizes the importance of sterilization in preventing contamination, disease spread, and maintaining the integrity of food, research, and industrial processes.