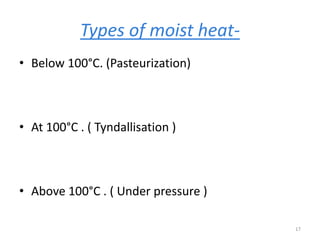
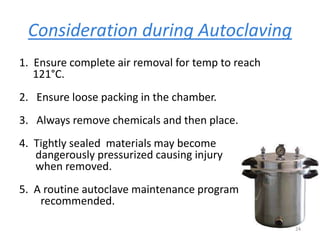
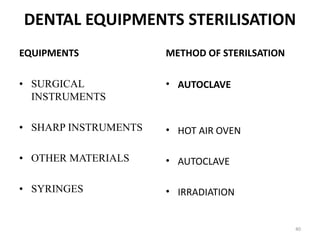
1. Physical agents such as heat, drying, filtration, and radiation can be used to sterilize materials. Moist heat via autoclaving at 121°C for 15 minutes is the most reliable method and kills all microorganisms including bacterial spores.
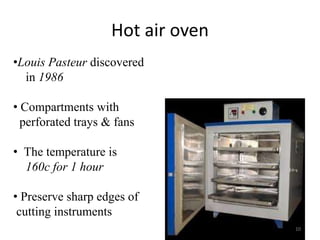
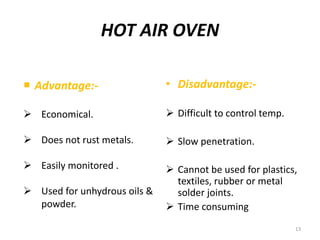
2. Dry heat via hot air ovens at 160°C for 1 hour can sterilize heat stable materials but has poor penetration. Filtration through membrane filters with 0.22μm pores is used to sterilize heat labile liquids.
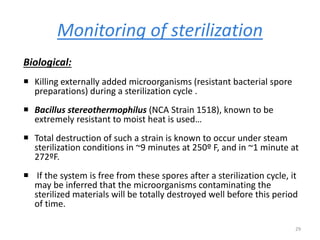
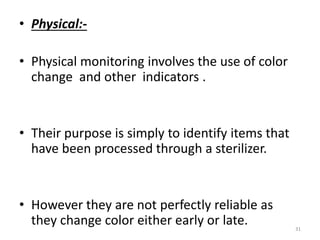
3. Proper monitoring of sterilization methods is important to ensure effectiveness using biological indicators of bacterial spores or chemical indicators that change color.





![1]FLAMING
2]INCINERATION
3]HOT AIR OVEN
7](https://image.slidesharecdn.com/sree-161116055449/85/Sree-7-320.jpg)