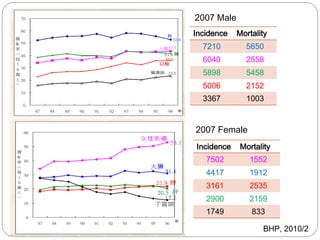
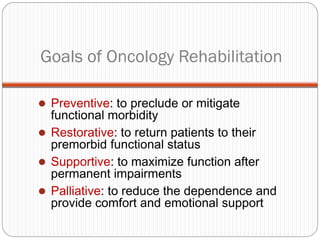
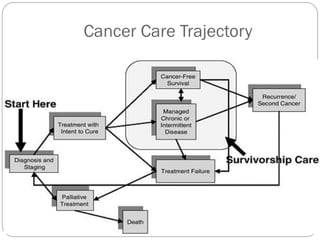
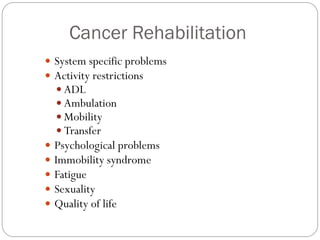
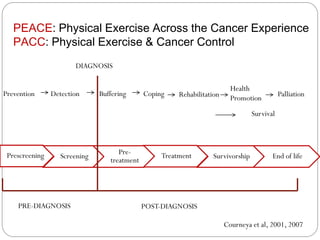
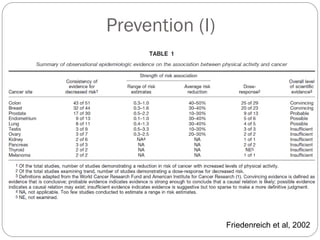
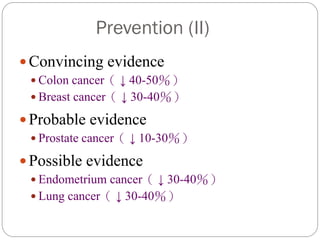
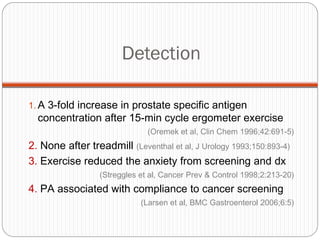
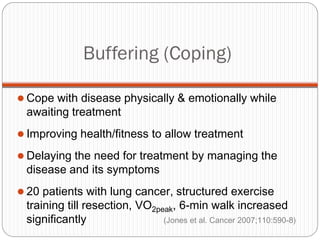
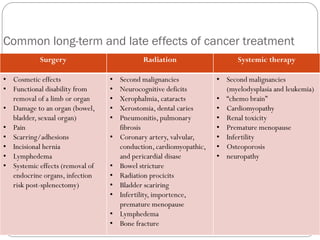
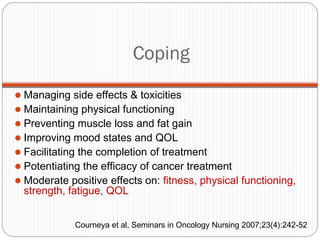
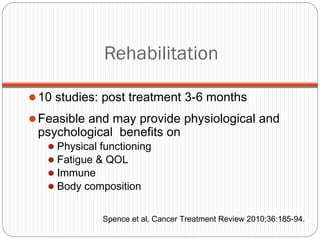
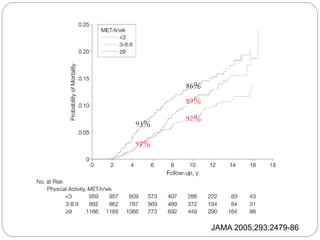
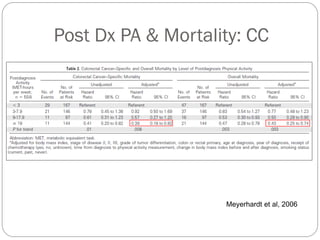
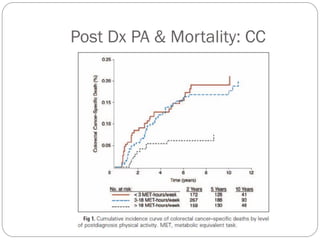
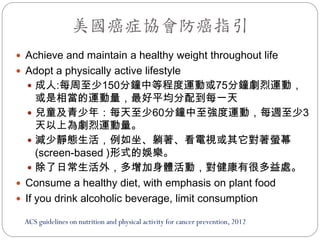
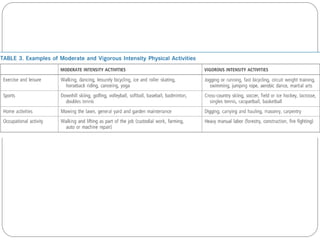
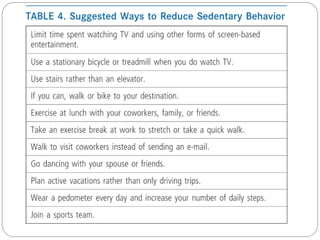
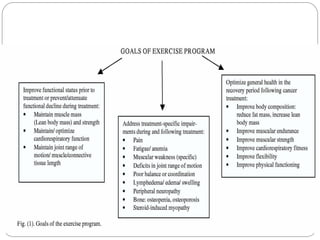
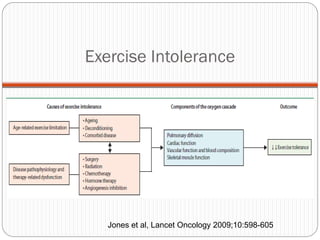
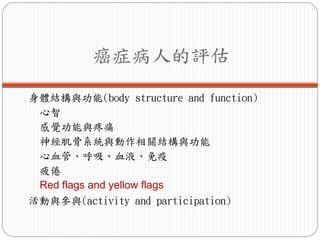
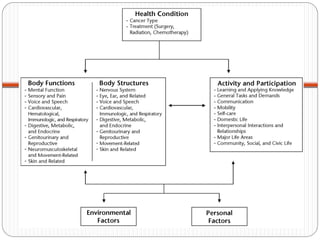
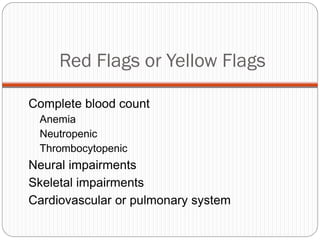
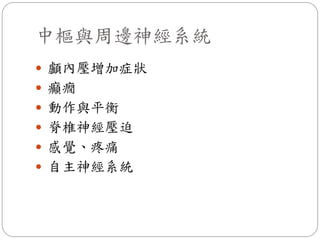
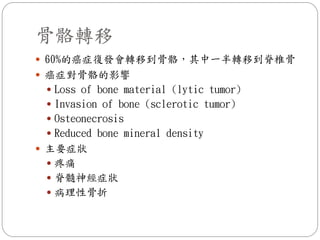
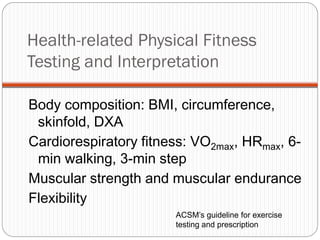
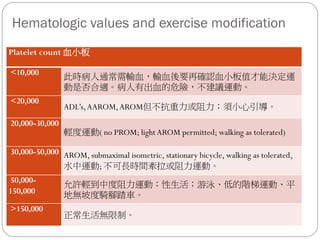
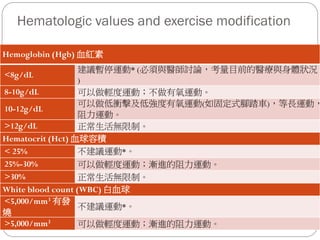
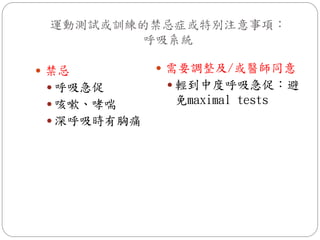
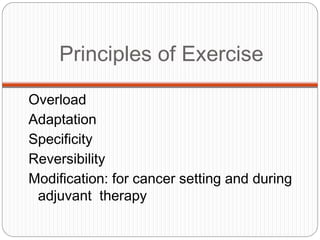
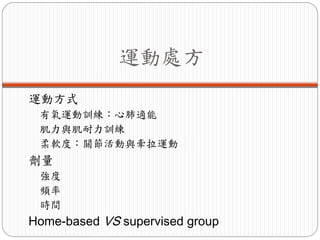
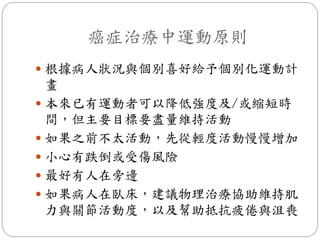
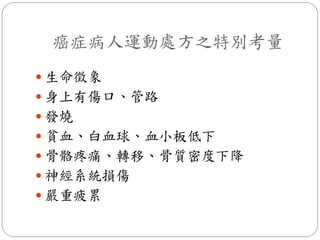
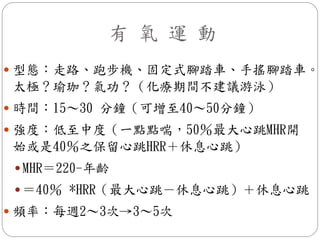
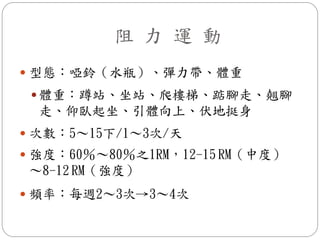
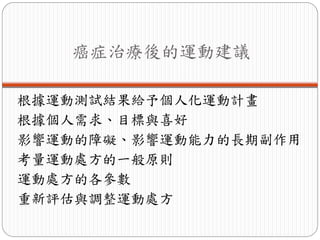
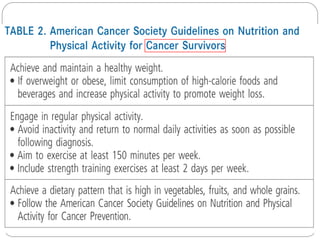
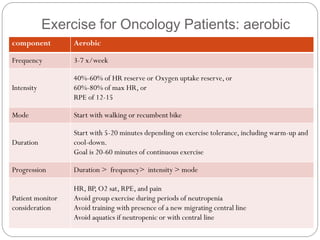
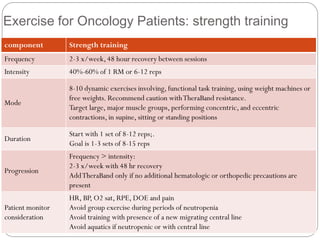
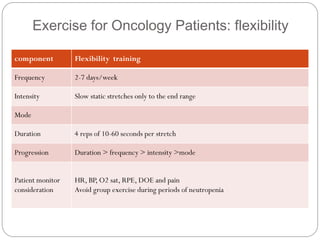
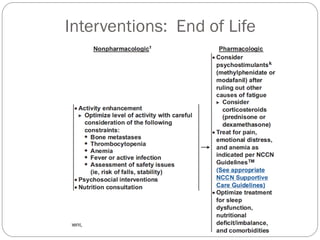
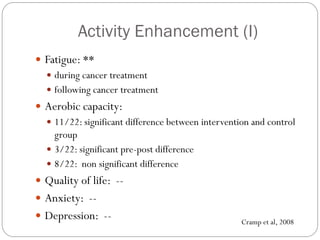
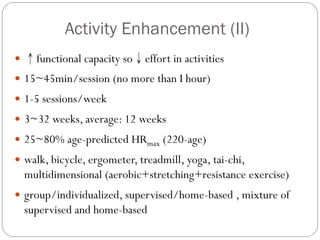
The document discusses exercise for cancer patients across the cancer care trajectory. It covers goals of cancer rehabilitation including prevention, restoration, support, and palliation. It then discusses exercise for prevention, detection, coping with treatment, rehabilitation after treatment, survival, health promotion, and palliation. Specific benefits of exercise discussed include reducing cancer risk and recurrence, managing treatment side effects, and improving physical and psychological well-being.