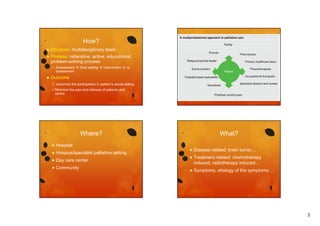
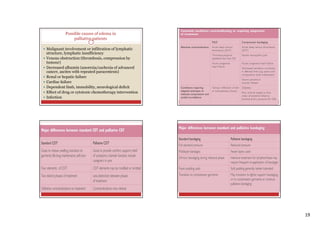
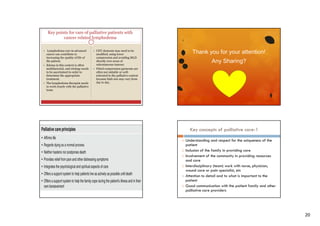
The document discusses palliative care, which aims to relieve suffering and improve quality of life for patients with serious illnesses. It provides an overview of palliative care goals, processes, interventions, symptoms addressed, and tools used to assess patients' physical functioning and set functional goals. The document also outlines examples of physical therapy interventions for common issues like pain, dyspnea, and fatigue in cancer patients.