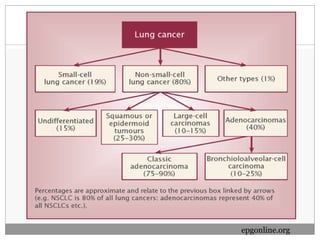
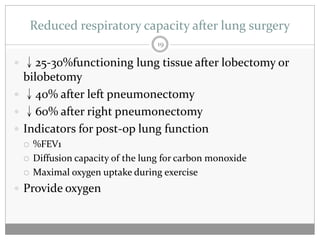
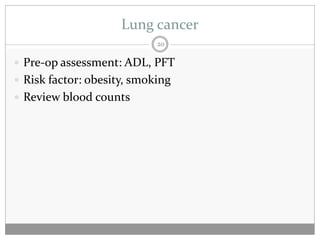
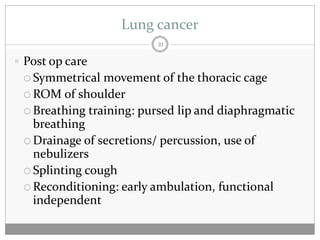
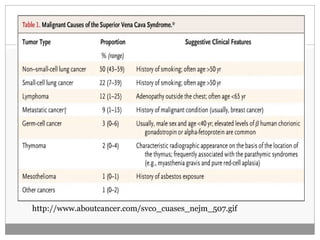
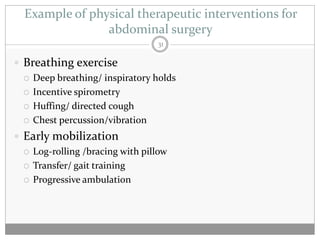
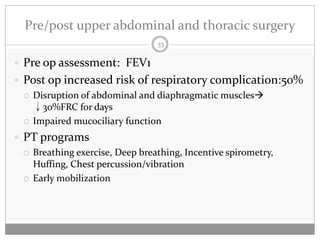
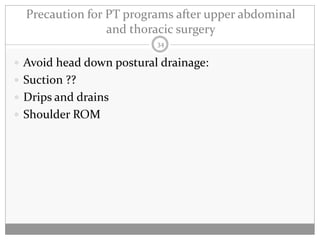
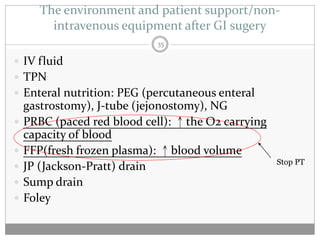
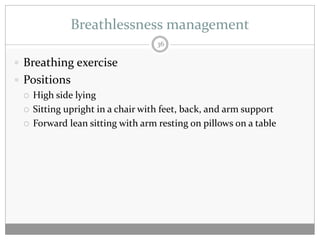
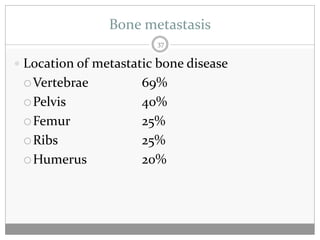
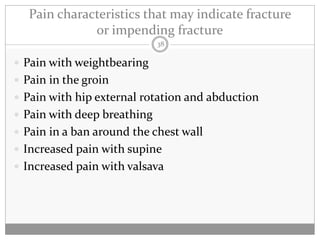
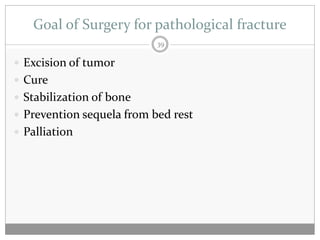
The document discusses physical therapy interventions for cancer patients after surgery, focusing on early mobilization, lung hygiene exercises, and specific rehabilitation programs for common cancer types like breast cancer, lung cancer, and gastrointestinal cancers. Post-surgery goals include preventing complications, improving range of motion, and managing symptoms like pain, breathlessness, and bone metastasis. Precautions and considerations for different surgeries are also outlined.