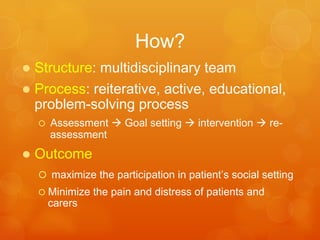
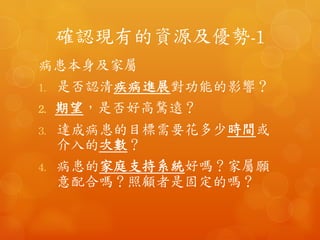
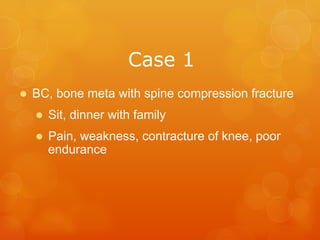
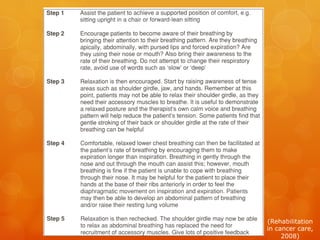
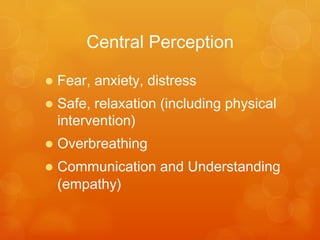
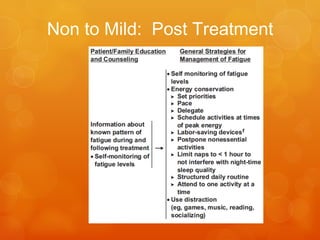
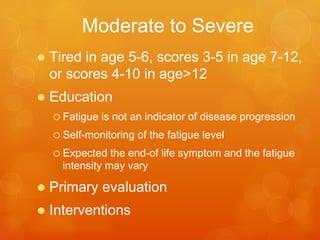
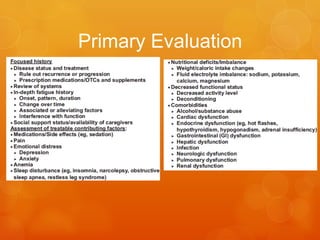
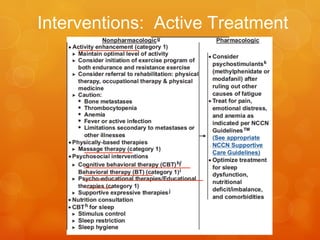
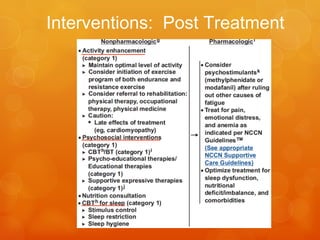
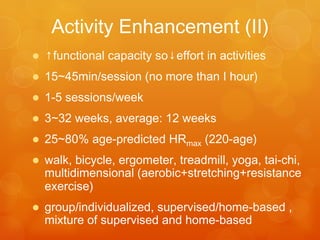
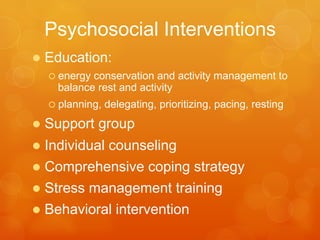
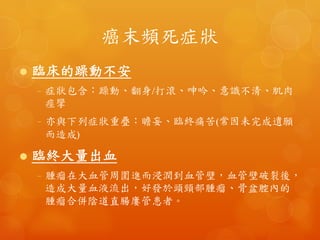
This document discusses palliative care, including its goals, focus, and methods. The goals of palliative care are to cure sometimes, relieve often, and comfort always. It focuses on maximizing quality of life for patients and their families by addressing physical and psychological aspects of disease and treatment. A multidisciplinary team conducts an iterative assessment and problem-solving process to establish goals and interventions. The goal is to maximize participation and minimize pain/distress for patients and caregivers. Common symptoms addressed include pain, breathing difficulties, fatigue, and mental health concerns. Assessment involves evaluating physical functioning, goals, resources, and developing individualized intervention plans.