This document summarizes various surgical procedures for strabismus, including:
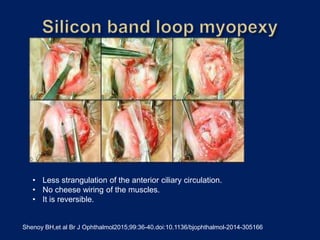
- Horizontal rectus muscle plication to shorten the muscle and strengthen it. Plication has advantages over resection such as preserving anterior ciliary circulation.
- Graded rectus muscle tenotomy and slanted recessions to correct strabismus in high myopia.
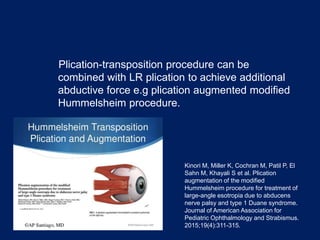
- Vertical rectus transposition to correct abduction deficiency in esotropic Duane's syndrome.
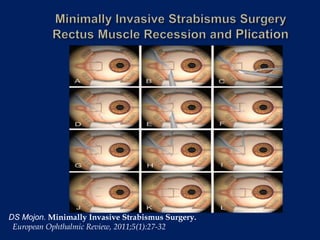
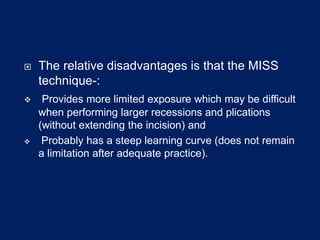
- Minimally invasive strabismus surgery techniques like MISS recession/plication which can be performed through a small incision.



























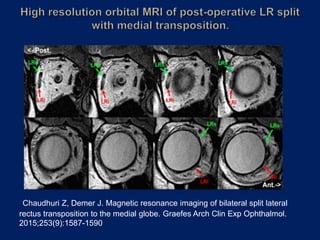
![ In 1991 Kauffmann introduced lateral rectus muscle splitting with
medial transposition for complete oculomotor palsy.
H. Kaufmann“Lateralis splitting” in total oculomotor paralysis with trochlear nerve paralysis
Fortschr Ophthalmol, 88 (1991), pp. 314–316 [in German]
He split the lateral rectus muscle and transposed its upper and
lower halves to the retroequatorial point, 20 mm from the limbus,
near the nasal superior and inferior vortex veins.
During the transposition procedure, he passed the upper half of
the lateral rectus muscle under the superior rectus muscle and
the lower half of the lateral rectus muscle under the inferior
rectus muscles.
Subsequently,Gokyigit et al presented a modification of this
technique by transposing the superior and inferior halves of the split
LR muscle anterior to the vortex vein and 2mm posterior to the
superior and inferior borders of the MR muscle.
Gokyigit B,Akar S,Satna B,Demirok A,Yilmaz OF.Medial transposition of a split lateral rectus
muscle for complete oculomotor nerve palsy.J AAPOS.2013;17(4):402-410](https://image.slidesharecdn.com/strabismus-191014053253/85/Strabismus-39-320.jpg)