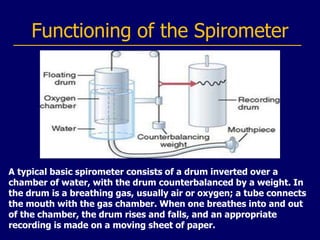
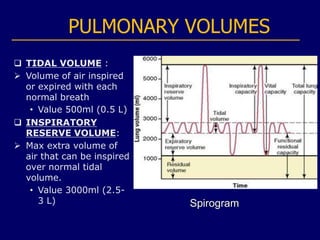
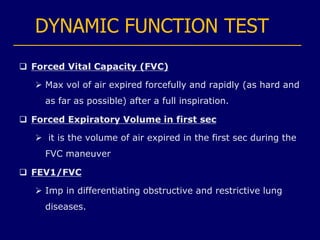
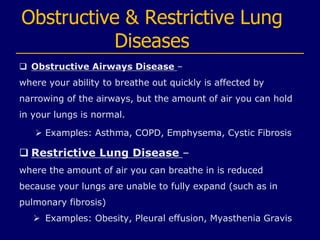
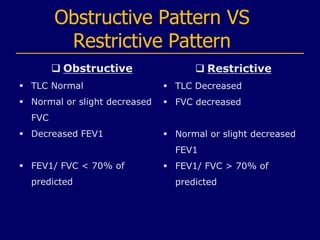
Spirometry is a common test used to assess lung function by measuring how much air a person can inhale and exhale. A spirometer is used to measure lung volumes like vital capacity and flows like forced expiratory volume. Spirometry can help diagnose and monitor conditions like COPD and asthma by identifying obstructive or restrictive lung patterns. The test involves forceful inhalation and exhalation into a mouthpiece for at least 6 seconds while seated in front of the spirometer. Spirometry results are used to evaluate lung capacity, airflow limitation, and response to treatment over time.