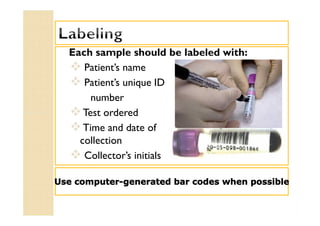
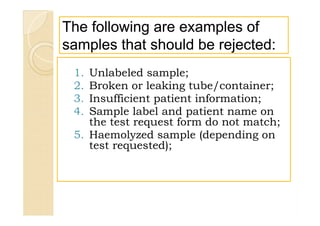
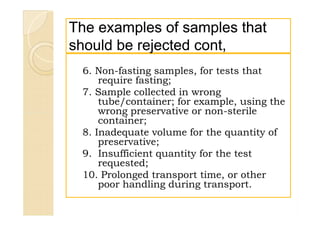
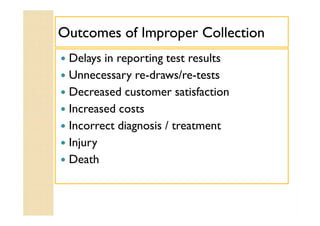
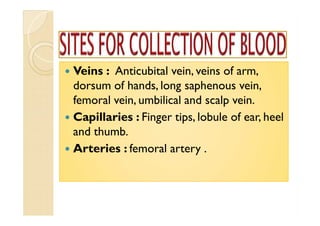
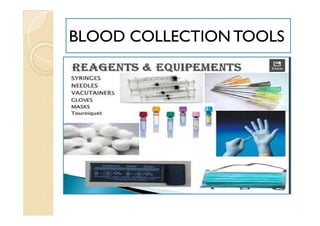
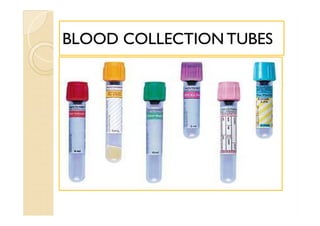
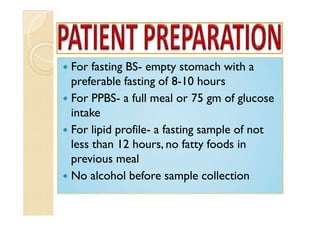
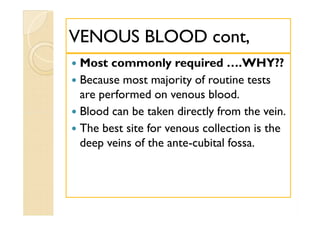
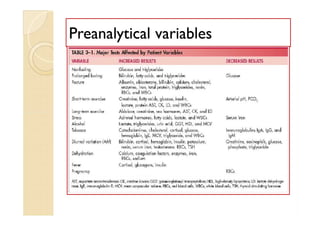
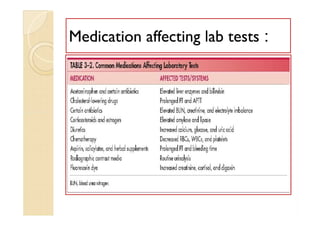
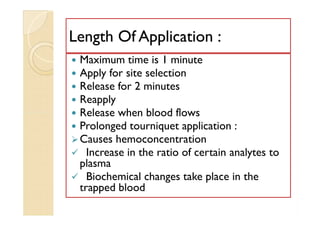
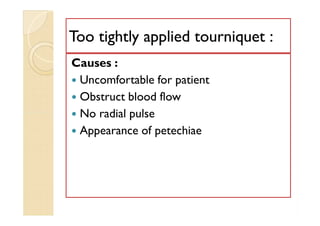
The document discusses proper sample management procedures for a laboratory. It emphasizes that sample quality directly impacts the accuracy of test results and patient care. Key aspects of sample management include detailed collection instructions, proper labeling, handling and transport of samples, criteria for rejecting unacceptable samples, and ensuring samples are collected according to testing requirements. Adhering to standardized sample management procedures helps produce reliable results and avoid errors.