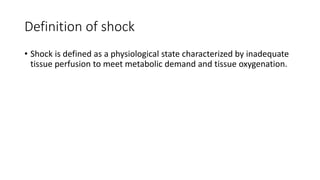
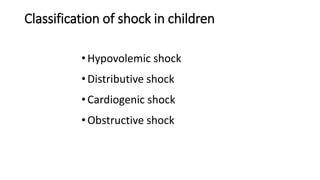
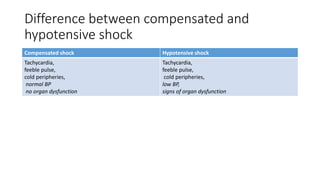
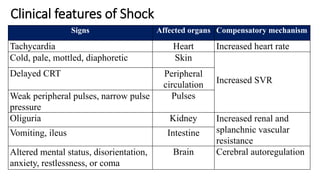
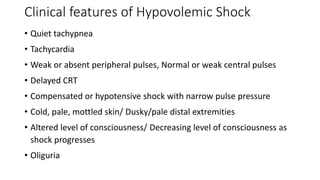
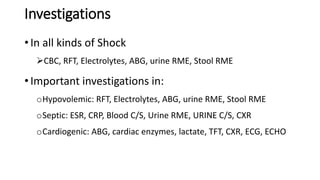
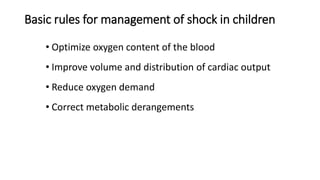
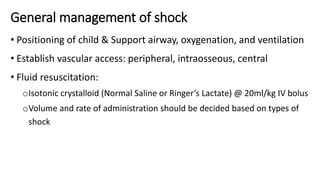
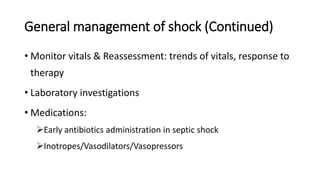
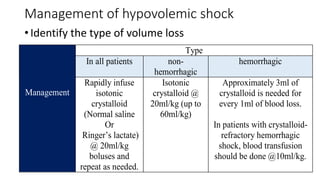
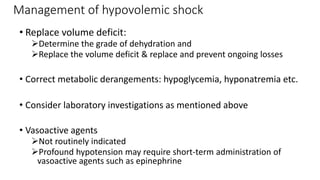
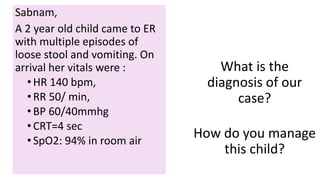
This 2-year old child presented with signs of hypovolemic shock including a heart rate of 140 bpm, respiratory rate of 50/min, blood pressure of 60/40 mmHg, capillary refill time of 4 seconds, and oxygen saturation of 94% in room air. The child is experiencing hypovolemic shock likely due to acute gastroenteritis leading to vomiting and diarrhea causing significant fluid loss. Management should include rapid intravenous fluid resuscitation with isotonic crystalloids such as normal saline, monitoring of vitals, laboratory tests to identify cause and guide management, and treating any metabolic derangements present.