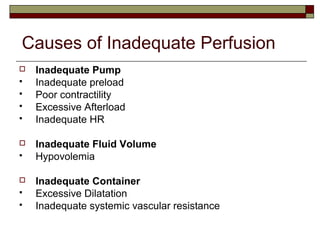
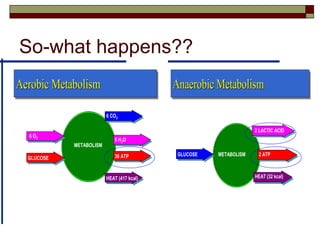
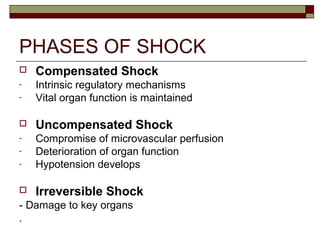
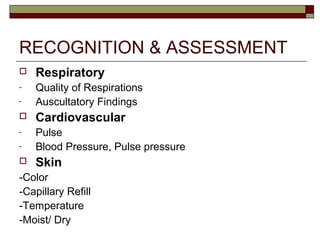
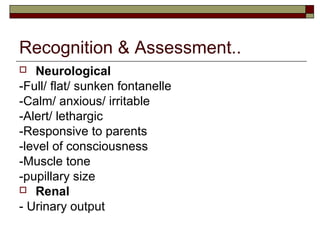
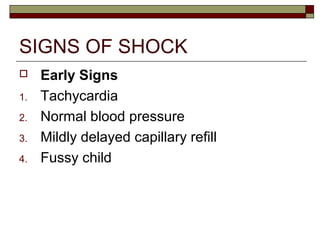
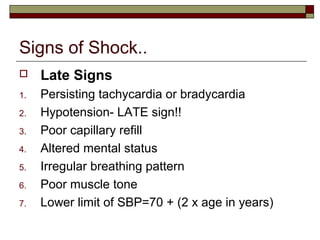
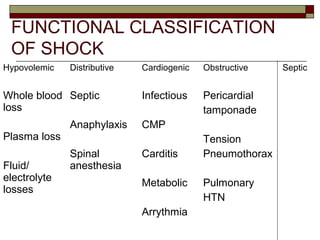
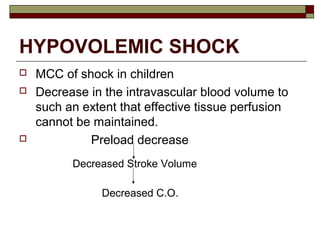
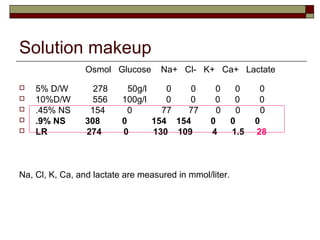
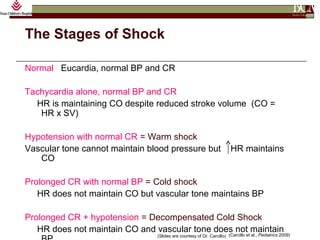
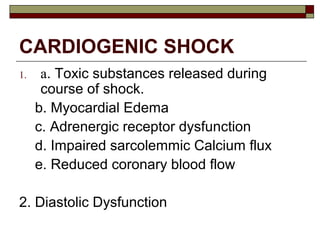
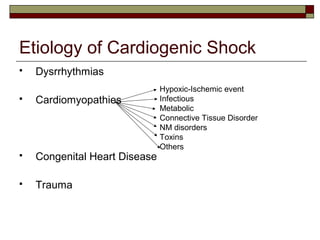
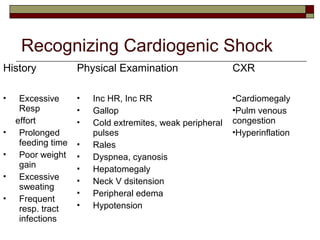
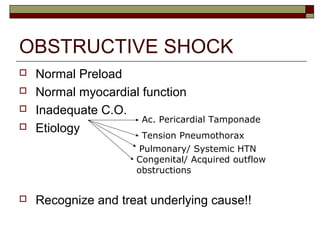
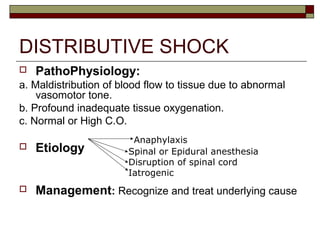
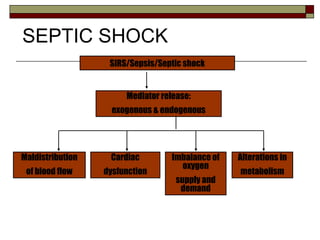
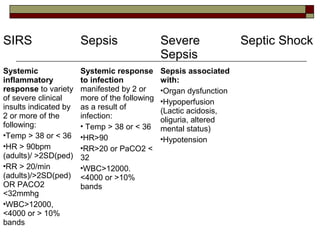
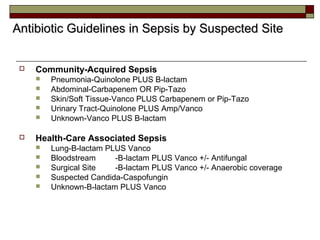
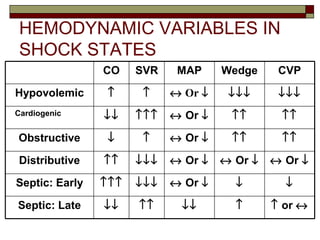
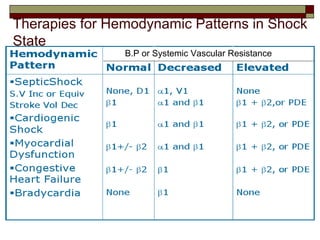
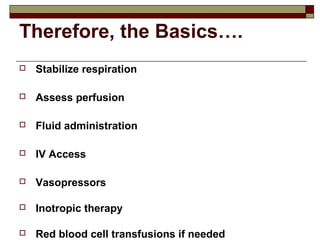
This document defines shock in children and discusses its physiology, classification, etiologies, recognition, assessment, and management. Shock is defined as an acute circulatory dysfunction resulting in insufficient oxygen delivery to tissues. The main types of shock discussed are hypovolemic, distributive, cardiogenic, obstructive, and septic shock. Signs of shock progress from early compensated stages to later uncompensated stages with declining perfusion. Management involves identifying and treating the underlying cause while stabilizing circulation through fluid resuscitation, vasopressors, and inotropes. Early goal-directed therapy is important for managing septic shock.