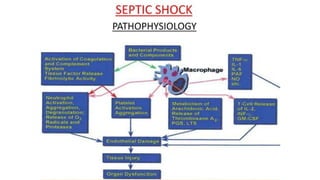
The document provides an overview of shock in children, defining it as a failure of the circulatory system to meet the metabolic demands of tissues, leading to various stages of shock. It details the causes, types, signs, pathophysiology, and treatment approaches for different types of shock, including hypovolemic, cardiogenic, septic, obstructive, and distributive shock. The emphasis is placed on early assessment and intervention to restore tissue perfusion and improve outcomes.