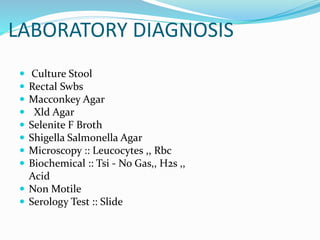
This document describes Shigella, the bacteria that causes bacillary dysentery. It is a gram-negative, non-motile, non-lactose fermenting bacillus. Shigella has four main species and causes acute bacterial infection of the intestine through invasion and various toxins. It spreads through the fecal-oral route and causes fever, bloody diarrhea, and abdominal cramps. Diagnosis involves microscopy and culture of a stool sample. Treatment depends on severity but may include antibiotics and prevention focuses on water, sewage, and food safety as well as personal hygiene.