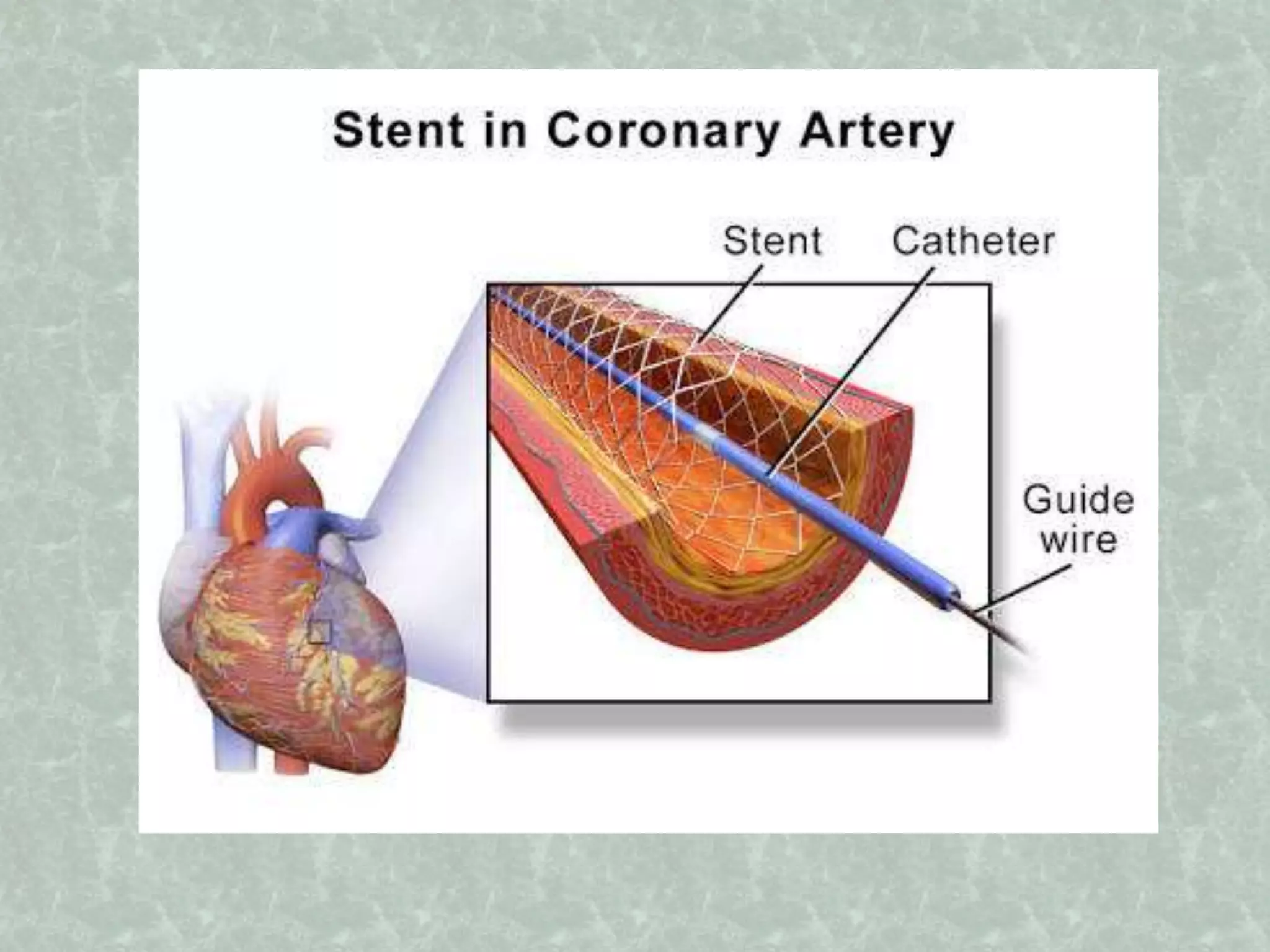
- Endovascular surgery uses catheter-guided devices to restore blood flow in occluded vessels by delivering thrombolytic agents directly to clots or removing clots mechanically.
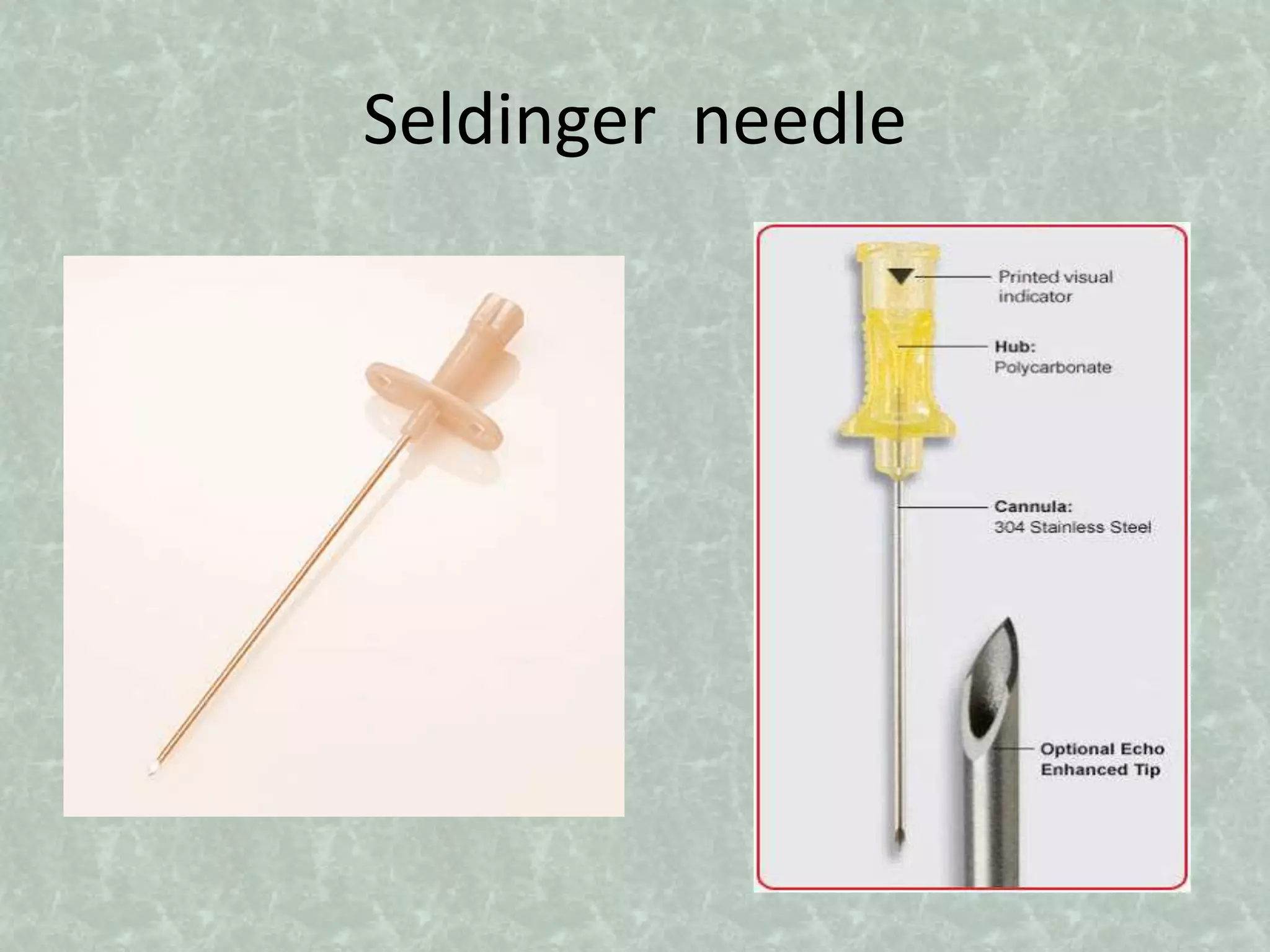
- The technique was pioneered in the 1950s-1980s through developments like the Seldinger technique for arterial access using guidewires, methods for extracting thrombus using balloon catheters, and introducing balloon angioplasty and stents.
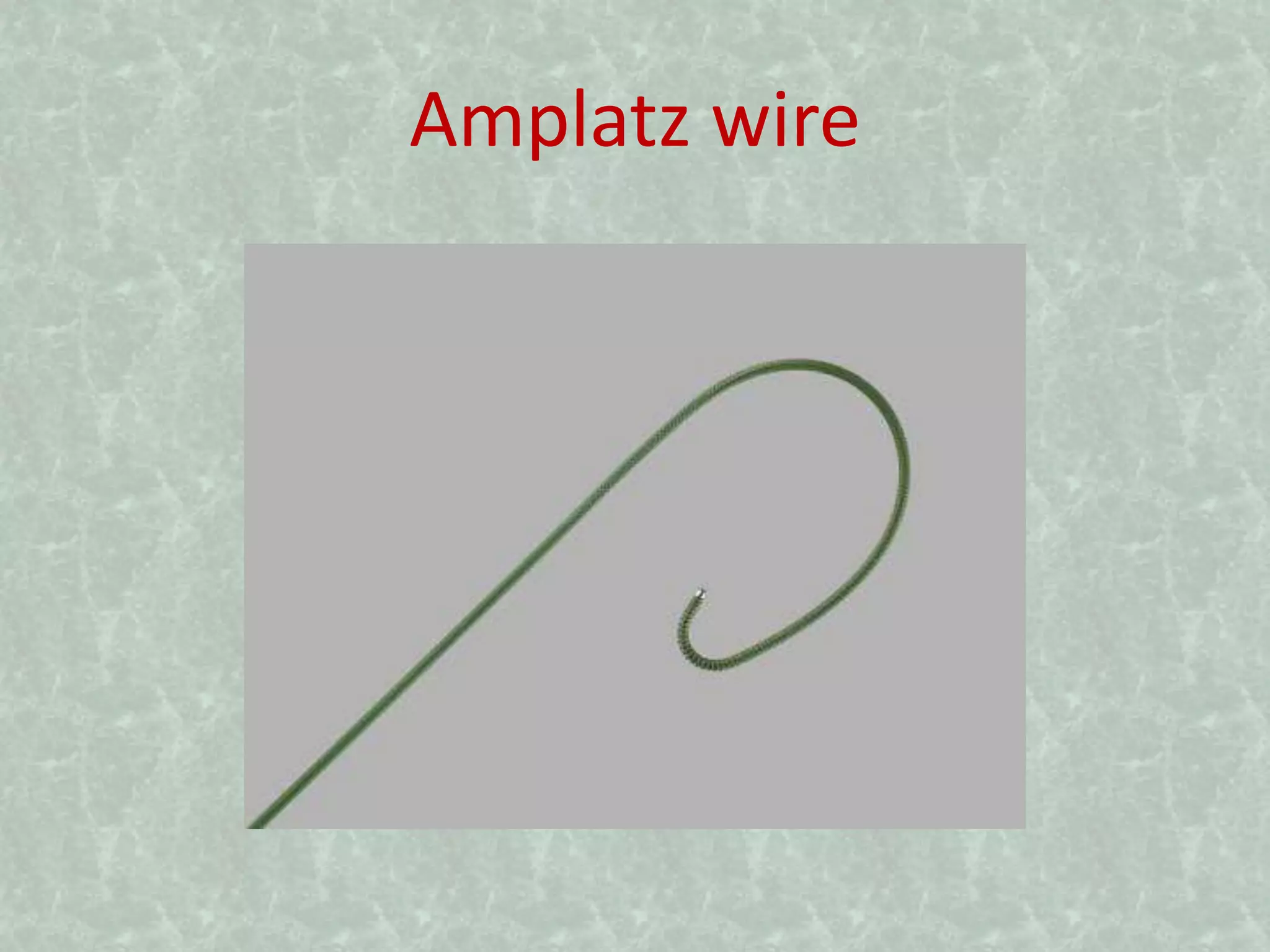
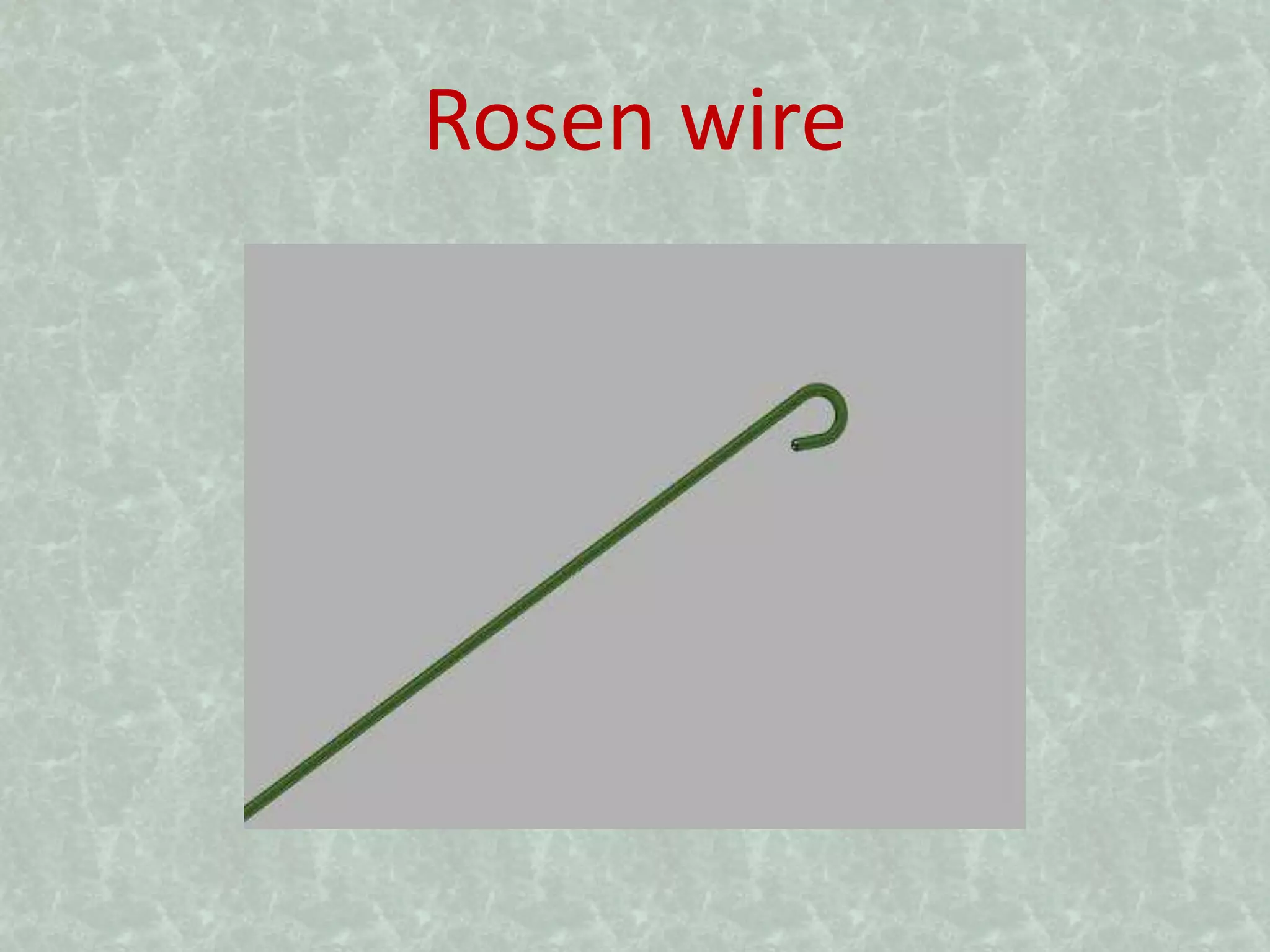
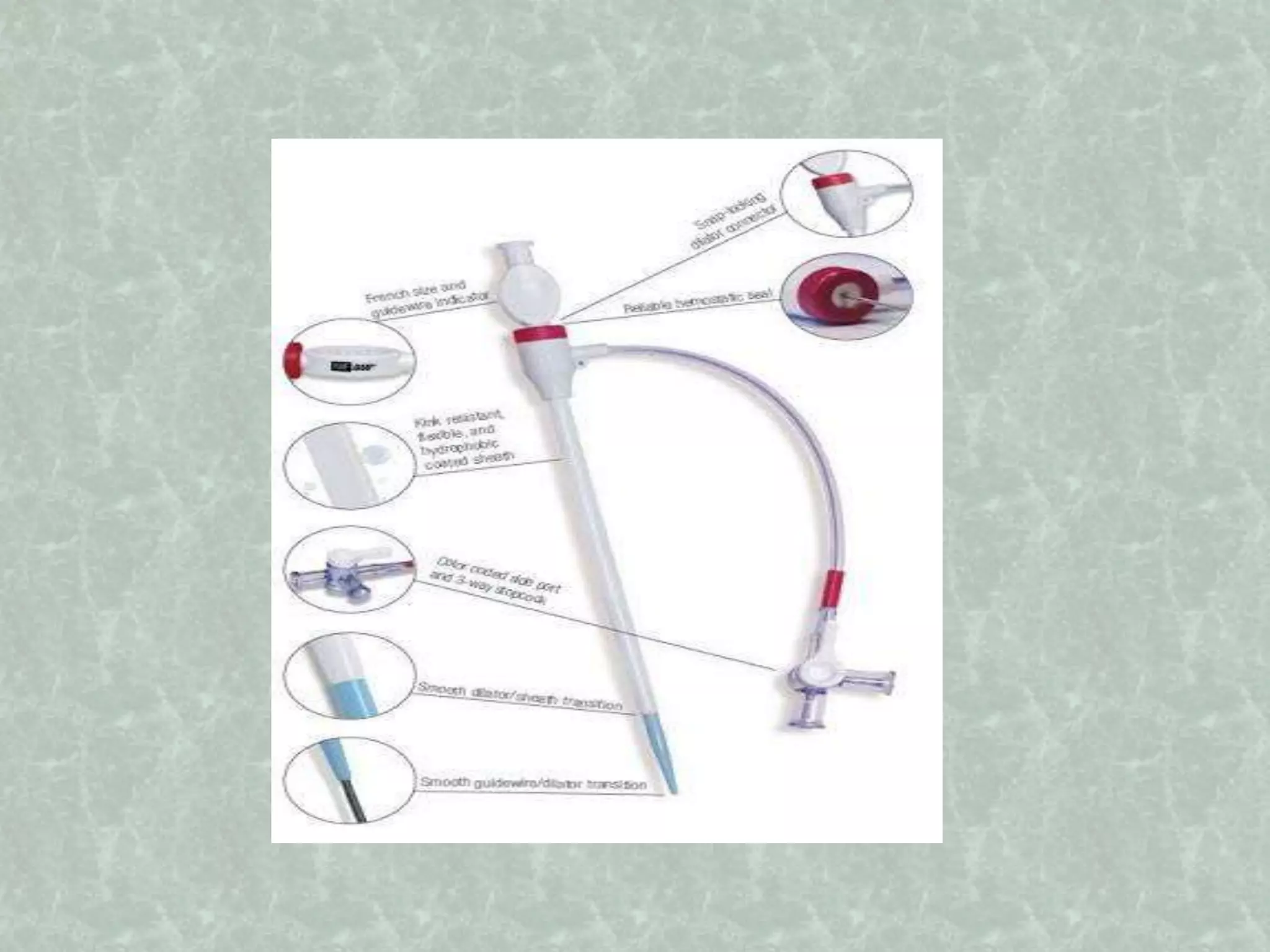
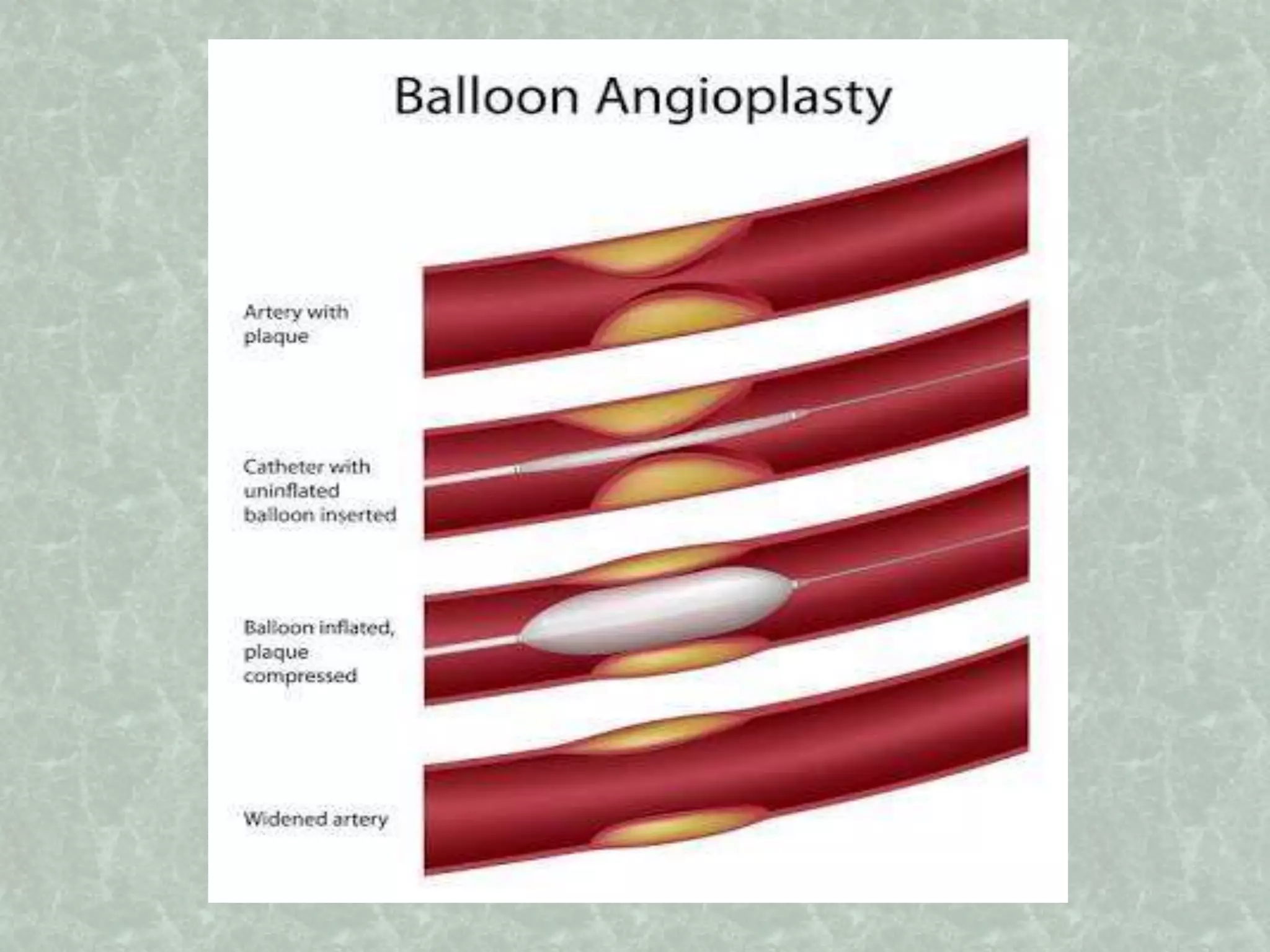
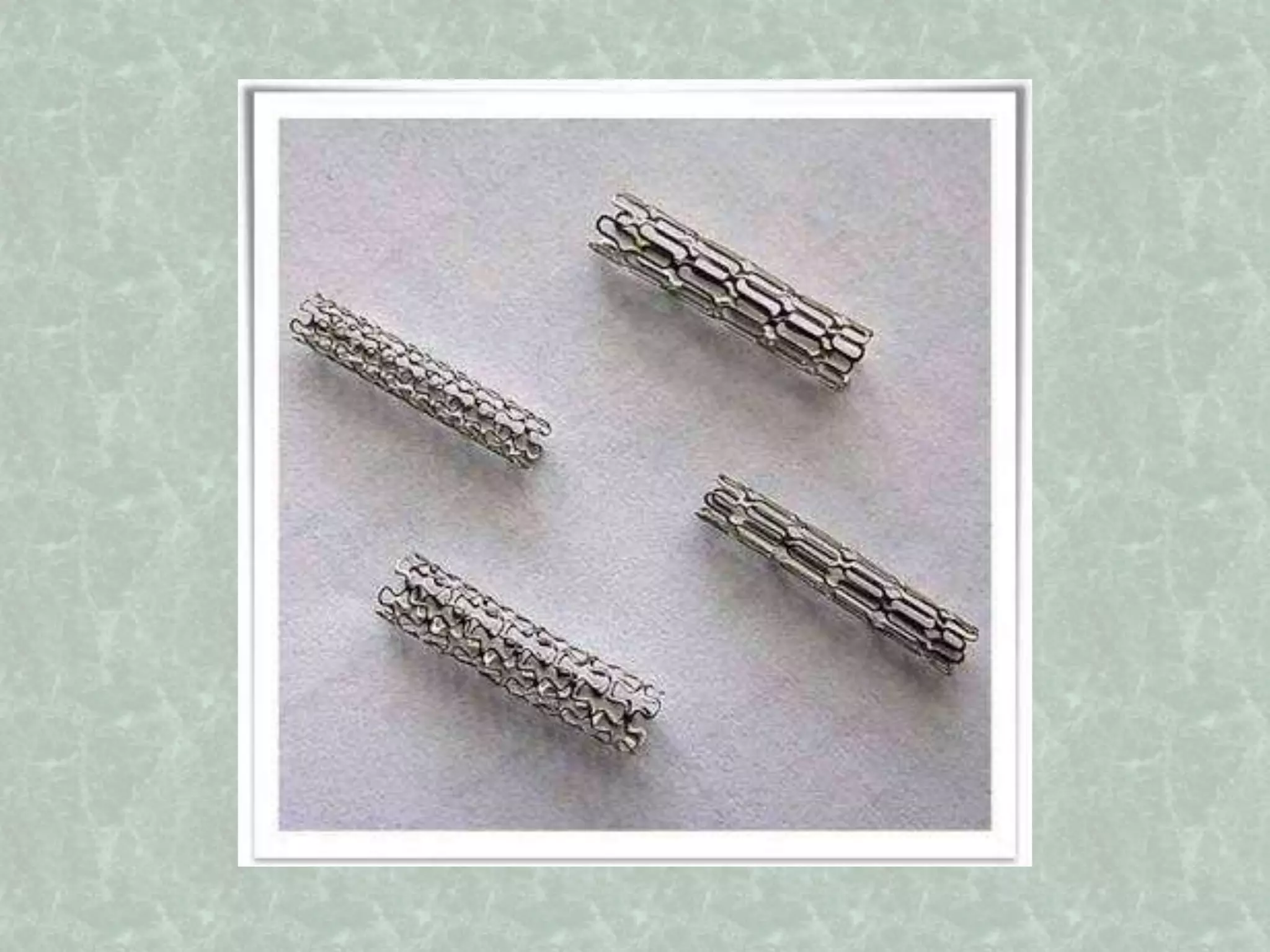
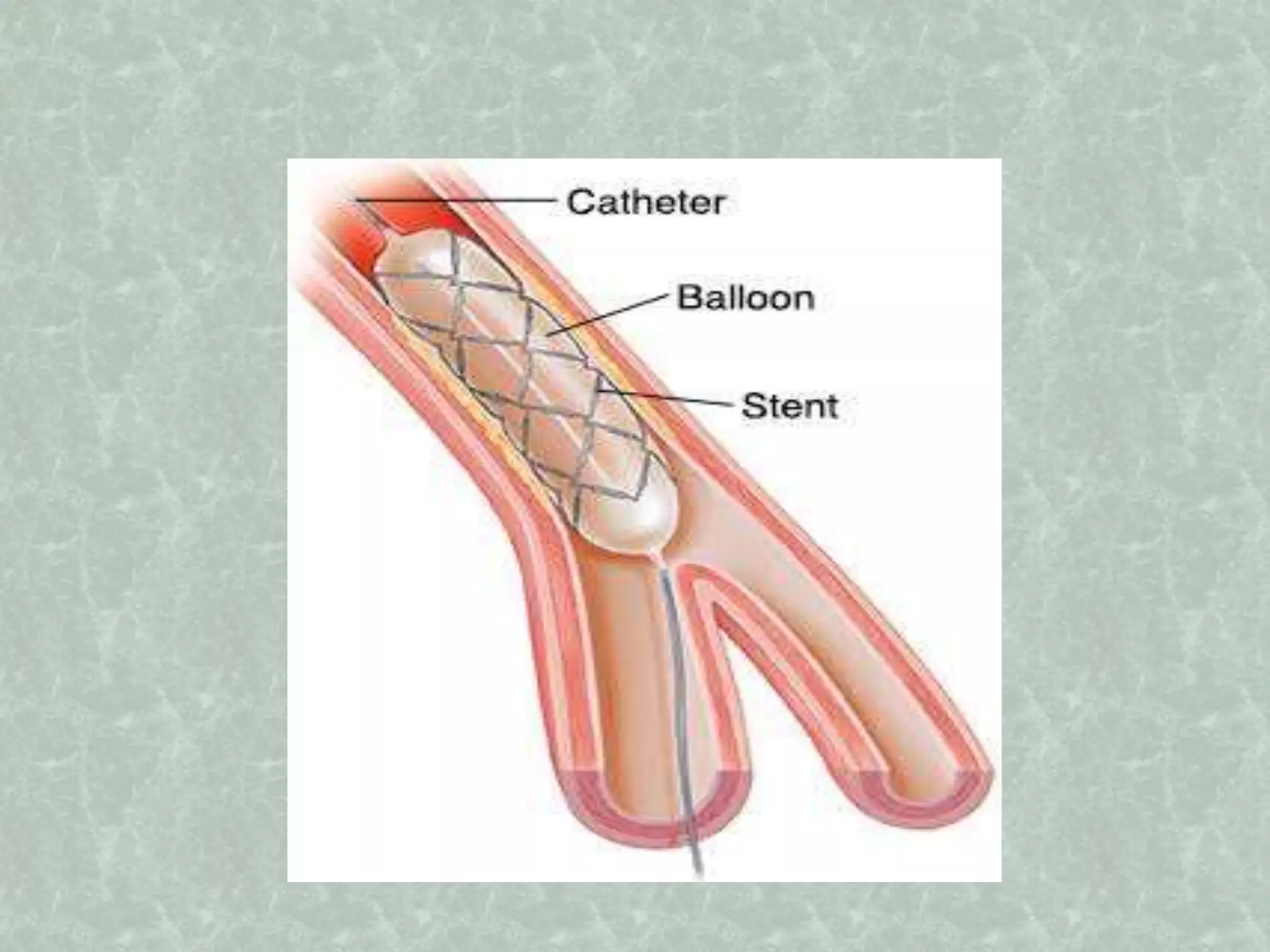
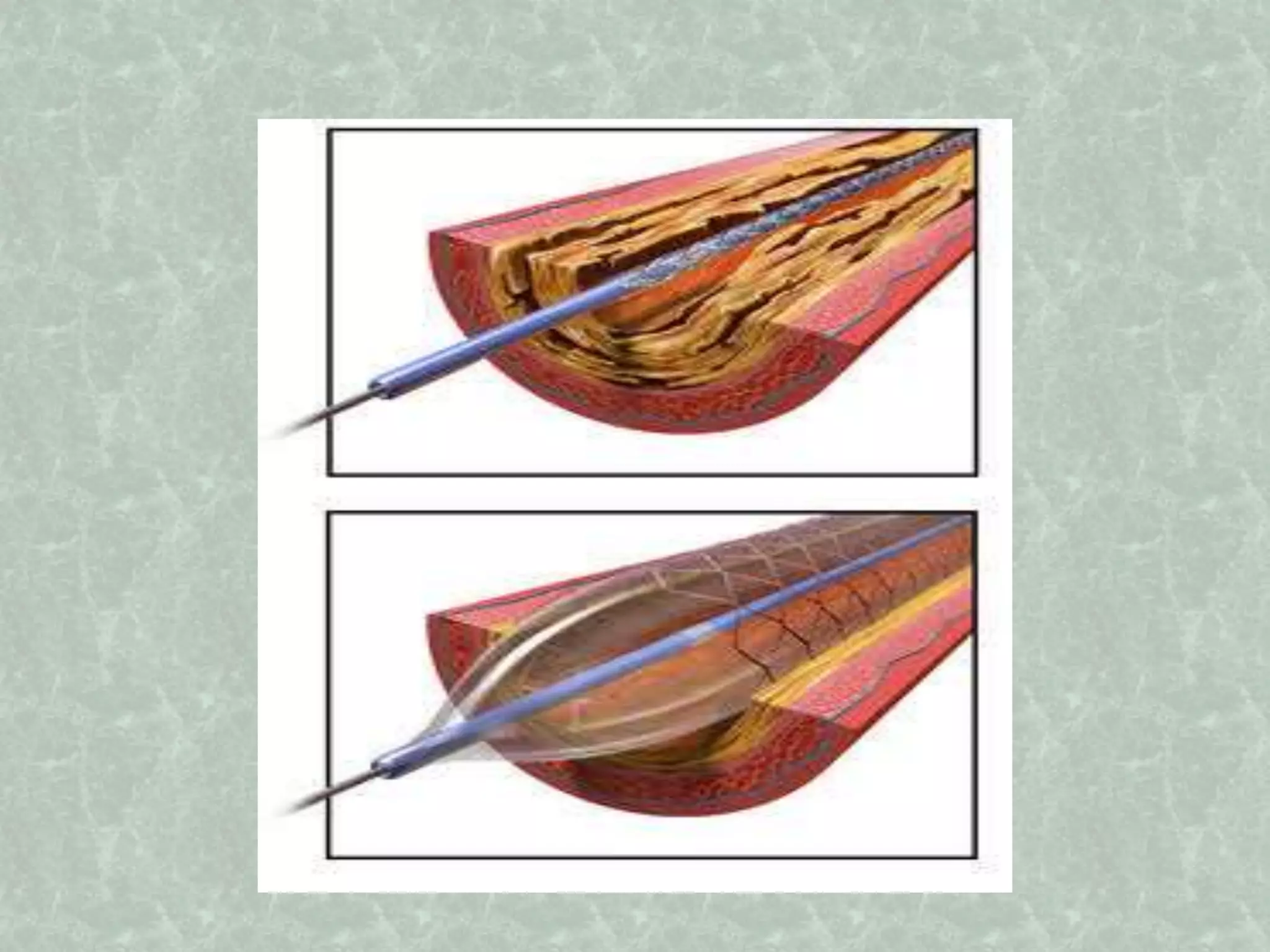
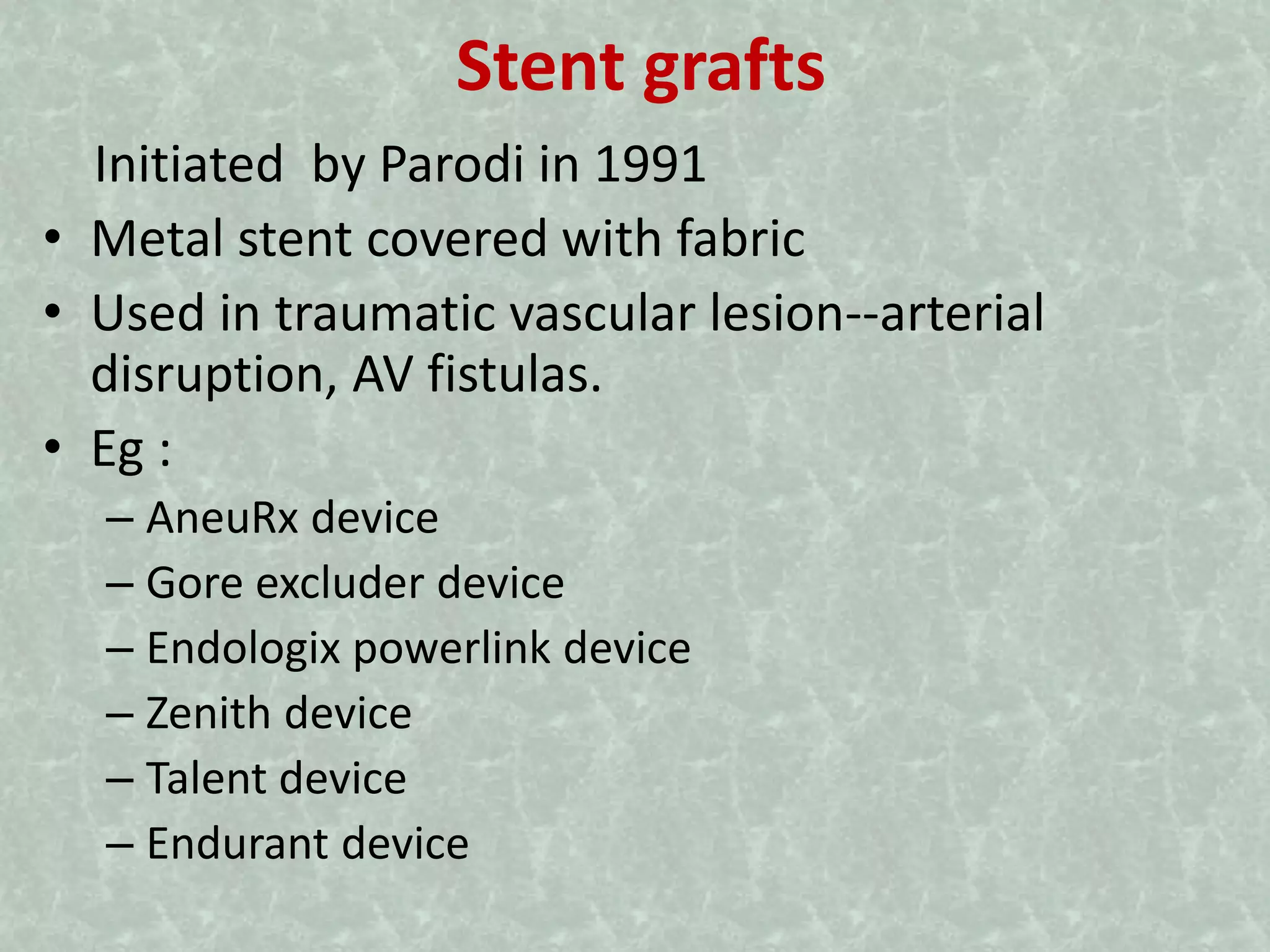
- Key devices used in endovascular procedures include guidewires, catheters, balloons, stents, and stent grafts, each with characteristics suited to their purpose like accessing vessels, delivering thrombolytic agents, dilating stenoses, scaffolding vessels, and excluding aneurys