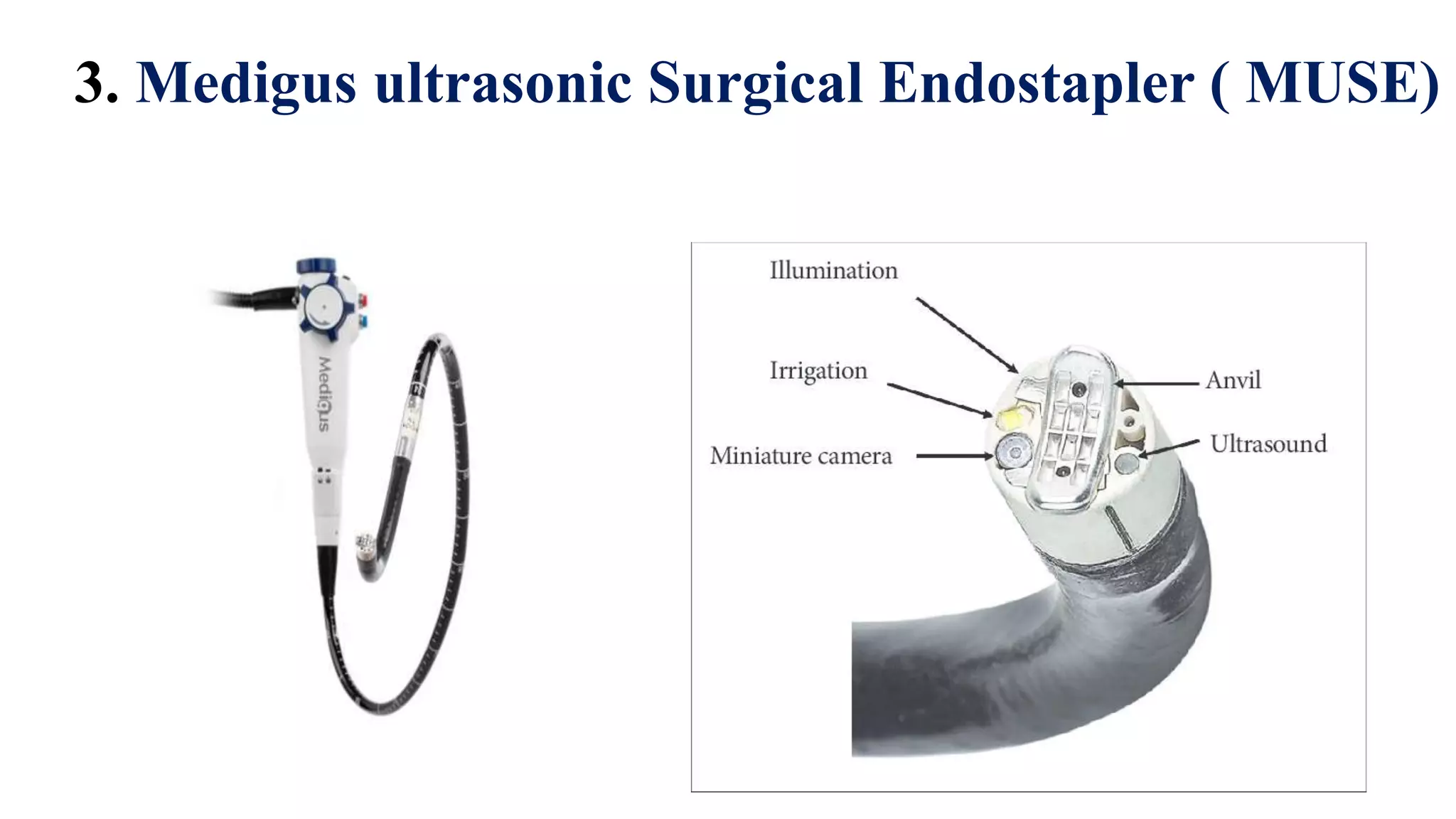
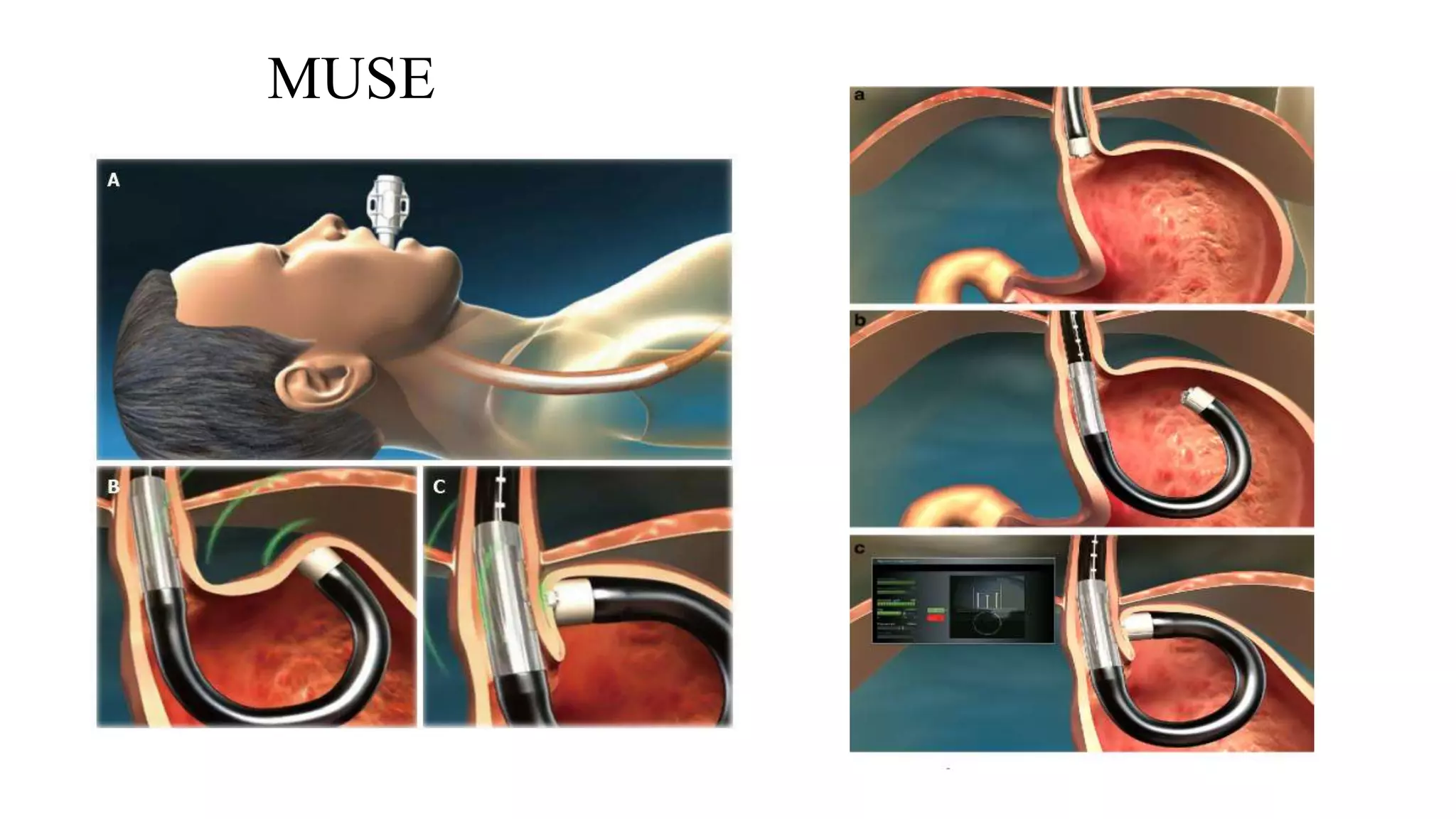
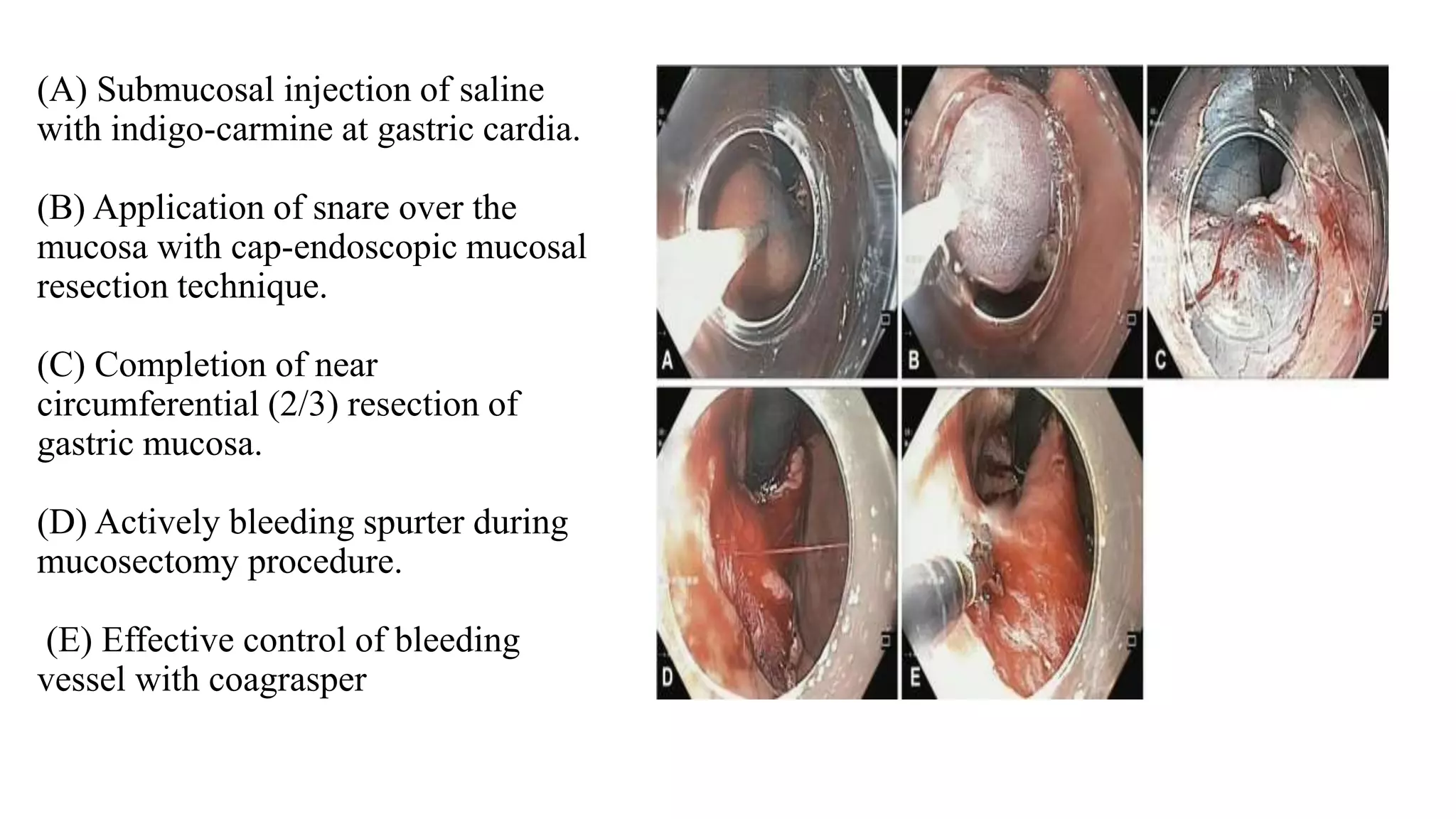
Dr. Biswajit Deka presented on endoluminal treatments for GERD. He discussed the pathophysiology of GERD and how endoluminal procedures aim to increase LES tone and length to prevent reflux. The main endoluminal procedures covered were EsophyX which creates an incisionless fundoplication, Stretta which uses RF to remodel the LES, MUSE which creates a partial fundoplication with staples, and injections or mucosal excision techniques. Complications were generally minor but include bleeding, perforation, and pain. Endoluminal GERD treatments are promising but still developing compared to anti-reflux